Do You See IUP?
Written by: Victor Bernal, DO. Edited by: Jeff Greco, MD
Case
A 38-year-old female, G6P3A2, with history of recent misoprostol use 3 weeks ago for a presumed ectopic pregnancy comes in for worsening abdominal pain over the last week. On her last visit to the ED, her beta-hCG had been appropriately trending down, with a last measurement 200 IU/L. Patient endorses mild vaginal spotting. History of 2 prior C-sections. VS are unremarkable in the ED. Luckily, you are on your favorite off-service rotation and have the time and luxury of doing a bedside ultrasound.
Differentials
Kidney Stone
Appendicitis
Diverticulitis
Constipation
Urethritis
PID
Ectopic Pregnancy
Retained Products of Conception
Ovarian Torsion
Ovarian Cyst
UTI
Choriocarcinomas
Subchorionic Hematomas
Assessing for IUP
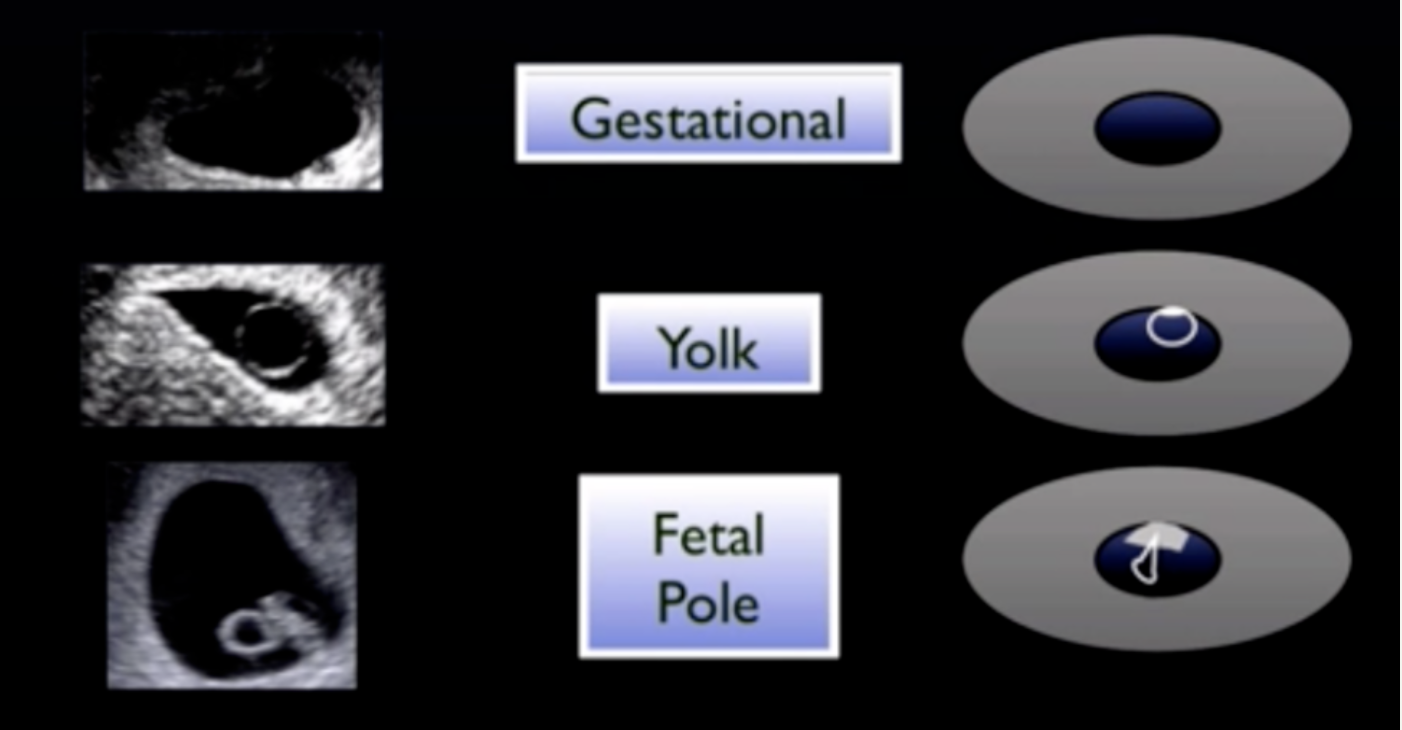
To effectively rule out an ectopic pregnancy (2% of all pregnancies) via ultrasound, an intrauterine pregnancy (IUP) must be visualized. This entails a yolk sac or fetal pole in a gestational sac within the uterus. As with all pregnancies, timing is everything! To assess for an IUP, one must take into account the type of POCUS...transvaginal versus transabdominal.
Figure 1: 1st Trimester Pregnancy Structures to Assess for IUP
Table 1: When One Can Visualize Structure with beta-hCG Levels
It is no surprise that transvaginal ultrasounds offer visualization of these structures sooner. However, in correlation with beta-hCG levels, one can still determine the presence of an IUP with a transabdominal US. Furthermore, if there is concern for a ruptured ectopic, the use of a curvilinear allows a physician to assess for free fluid in the RUQ area of Morrison’s Pouch, which has a PPV of almost 100%.
Caveats
Heterotopic Pregnancy - Just because you see an IUP, does not mean that there cannot be another gestation outside the uterus. With the advent of in vitro fertilization (i.e. IVF), cases of heterotopic pregnancies have risen dramatically. In this case, a bedside US showed a questionable fetal heart rate with cystic mass surrounding the “flickering” structures. The sonoteam scratched their heads as to what it could be. TVUS showed a questionable caesarean section ectopic versus retained products of conception. The patient is currently scheduled for a definitive D&C to remove such products. There have been further case reports of placental site trophoblastic tumors and choriocarcinomas from prior C-sections. Although most of these patients are stable, this should raise the question of further management, as these patients are prone to coming back. Definitive management lies in surgical treatment by OBGYN. It is appropriate to keep these new differentials on the list as IVF and C-sections become more common.
Conclusion
POCUS is a great, easy tool to assess for pregnancy viability, although timing is everything. Knowing your limitations is key as pregnancies may not be visualized at 3-5 weeks. Furthermore, US is user dependent.
When assessing a child-bearing age female with lower abdominal pain, keep the differential broad, as you may never know what you may encounter.
Always assess for risk factors, including prior C-sections and IVF
Citations
Bekci T, Ozturk M, Danaci M. Caesarean Scar Choriocarcinoma: Ultrasound and Magnetic Resonance Imaging Findings. J Belg Soc Radiol. 2016
Condous G, Kirk E, Lu C, et al. Diagnostic accuracy of varying discriminatory zones for the prediction of ectopic pregnancy in women with a pregnancy of unknown location. Ultrasound Obstet Gynecol 2005; 26:770.
Doubilet PM, Benson CB, Bourne T, Blaivas, M. Diagnostic Criteria for Nonviable Pregnancy Early in the First Trimester. Ultrasound Q. 2014; 30(1):3–9.
Gurung G, Amatya A, Thakur N, Rana A. Placental site trophoblastic tumor with perimetrial invasion and cesarean scar perforation (A case report) Nepal Journal of Obstetrics and Gynaecology. 2008;3:55–7.
Johns J, Greenwold N, Buckley S, et al. A prospective study of ultrasound screening for molar pregnancies in missed miscarriages. Ultrasound Obstet Gynecol 2005; 25: 493–497.
Moore C et al. Free fluid in Morison's pouch on bedside ultrasound predicts need for operative intervention in suspected ectopic pregnancy. Acad Emerg Med. 2007; 8:755-8.
Qian ZD, Zhu XM. Caesarean scar choriocarcinoma: a case report and review of the literature. Eur J Med Res. 2014;19:25. doi: 10.1186/2047-783X-19-25.