Lung Point Mimics
Written by: Aurora Jin, MD, Edited by: Jeff Greco MD
Background:
Ultrasound has been used in the diagnosis of pneumothorax in the emergency room for many years and has been shown to have superior sensitivity compared to chest X-ray. The “lung point” sign, in particular, is classically regarded as pathognomonic of pneumothorax, with studies citing up to 100% specificity. The lung point is visualized on ultrasound when a clear junction between two areas of lung with present and absent pleural sliding is identified in the same image. However, more recent research has established that lung point can be seen in other conditions, both physiologic and pathologic. Thus, it is important to be aware of lung point mimics before reaching for your chest tube tray.
US Findings:
● Ideally, use the high-frequency linear probe when evaluating for pneumothorax. Orient the probe perpendicular to the chest wall with the probe marker towards the patient’s head.
● Scan the areas of the chest where you would expect air to rise, i.e. the anterior chest wall (in a supine patient) or the lung apices (in an upright patient).
● Lung sliding can be seen as movement/shimmering of the pleura, described as “tiny marching ants.”
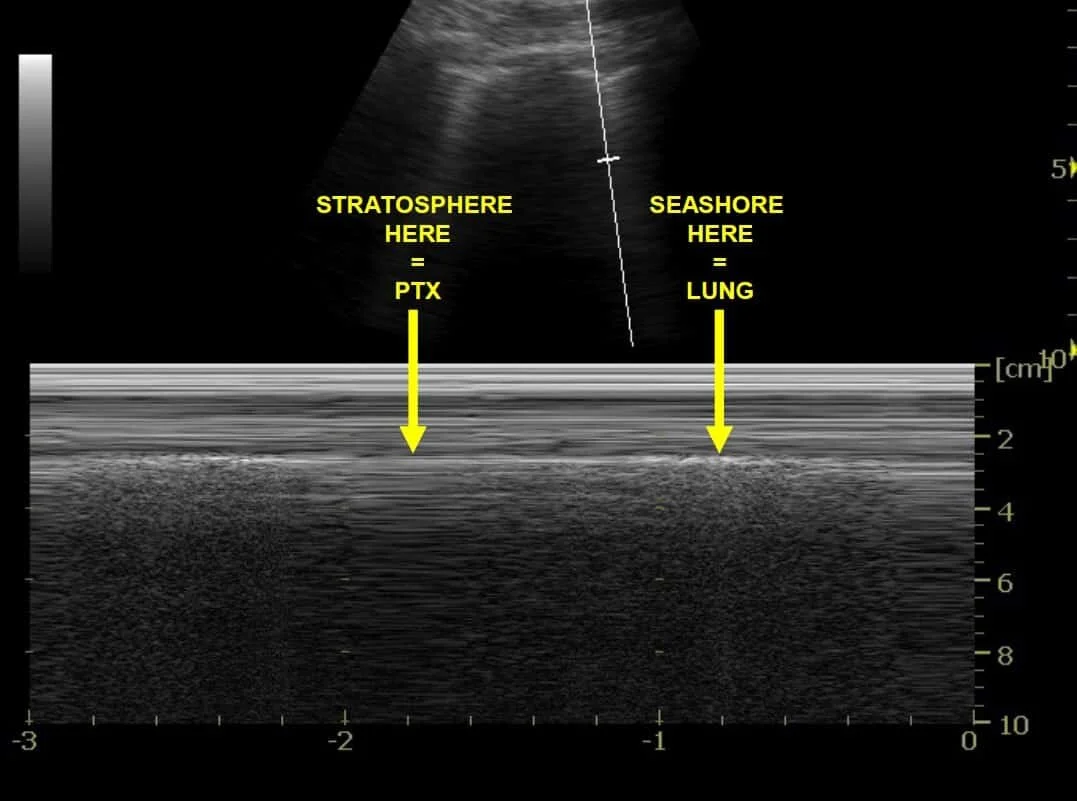
● With M-mode, properly inflated lung is confirmed with the “seashore sign,” where pleural movement is seen as the grains of sand, and the more superficial subcutaneous tissue anterior to the pleura is the water.
● If there is a pneumothorax, lung sliding will be absent.
● With M-mode, pneumothorax is suggested by “barcode/stratosphere sign,” which shows absence of movement both superficial and deep to the pleural line.
Figure 1 & 2: Lung point on B-mode (left); Lung point on M-mode (right).
Mimics:
Bullae
● Pulmonary bullae are defined as permanent areas of air trapping within the lung parenchyma that are ≥1cm in diameter. They are most classically seen in patients with a history of COPD/emphysema from tobacco smoking, although there have also been associations with marijuana smoking, vaping, IV drug use, and HIV.
● When the bulla extends completely superficially to the level of the pleura, a lung point may be visualized between the junction of normal lung tissue and the bulla. This lung point is sonographically identical to a true lung point from a pneumothorax.
Figure 3: Lung ultrasound of a patient with COPD showing what appears to be a lung point on M-mode with both seashore and barcode sign present (white arrow).
Figure 4: Subsequent CT demonstrated a large right-sided bulla.
Interstitial lung disease (ILD)
● ILD may lead to poor lung movement in affected areas due to pleural thickening, fibrosis, and/or adhesions.
● Thus, the transition point between healthy and diseased lung may appear as a lung point due to diminished pleural sliding; however, depending on the nature/extent of lung disease, other sonographic features of aerated lung may still be present (e.g. sliding A-lines, comet tails/B-lines), which can help to exclude pneumothorax.
Figure 5: Lung ultrasound demonstrating an area of seemingly absent (yellow arrow) and present (green arrow) lung sliding. A single isolated B-line (yellow asterisk) suggests that aerated lung is still present. Subsequent application of M-mode showed alternating barcode sign (yellow asterisk) and seashore sign (green asterisk). CXR and CT showed signs of pleural thickening and adhesions characteristic of asbestosis (red arrows).
Pulmonary contusion without associated pneumothorax
● Pulmonary contusion occurs after blunt trauma and is associated with destruction of the lung parenchyma and alveolar hemorrhage.
● Contused lung may also appear to lack pleural sliding on ultrasound; however, as with ILD, features such as sliding A-lines & comet tails/B-lines may still be present
● You may also see pleural discontinuity and lung parenchyma that appears more hypoechoic, which may indicate an isolated area of contused lung. These findings are not typical of isolated pneumothorax.
● In addition, you will usually not see a true barcode sign over a pulmonary contusion.
● However, a patient with chest trauma causing pulmonary contusion is also more likely to have an associated pneumothorax, so extra care must be taken to evaluate for both.
Figures 6, 7, & 8: Figure 6 (top): Lung ultrasound showing possible lung point (arrow) with comet tails on the left and movement with respiration (A » B). There is an area of pleural discontinuity with hypoechoic lung tissue deep to it, suggesting a possible area of contusion. Figure 7 (left):Subsequent application of M-mode showed rhythmic alternation of seashore sign (arrow) with lung point movement; however, true barcode sign was absent. Figure 8 (right): CT showed right-sided lung contusions without an associated pneumothorax.
Mediastinal and diaphragmatic junctions
● The junctions between lung and either the mediastinum or the diaphragm can be mistaken as lung point if, for example, the area of the chest being scanned is too close to these junctions, or identifying features of the heart/diaphragm/spleen/liver are not immediately apparent secondary to decreased image depth.
● Absence of A-lines and comet tails/B-lines can indicate that lung tissue is not present, and increasing your depth can help confirm whether you are scanning too close to the mediastinum or diaphragm.
● In addition, movement of the mediastinal pleura with the cardiac cycle may be observed, both in B-mode and M-mode.
Figure 9 (a&b): Application of M-mode over a possible lung point showing a cardiac pulse waveform (CP) over the area of concern, suggesting a false lung point at the lung-mediastinal junction. Subsequent CT ruled out pneumothorax.
Conclusion:
Lung point does not always signify pneumothorax. To avoid falsely interpreting a lung point as such, be aware of lung point mimics and their typical ultrasound findings. In addition, always correlate your clinical suspicion with other aspects of your patient’s case: physical exam, other imaging, case circumstances, and/or any past medical history.
References:
Thoracic and other images. Critical Care Northhampton.com: Reviewing Critical Care, Journals, and FOAMed. https://criticalcarenorthampton.com/thoracic-other-images/. Accessed 28 Jul 2021.
Bowra J. Lung ultrasound. Intensive Care Network. 2021. https://intensivecarenetwork.com/lesson/lung-ultrasound-pre-reading-for-fcus-course/. Accessed 28 Jul 2021.
Lichtenstein D, Mezière G, Biderman P, Gepner A. The “lung point”: an ultrasound sign specific to pneumothorax. Intensive Care Med. 2000 Oct;26(10):1434-40.
Ding W, Shen Y, Yang J, He X, Zhang M. Diagnosis of pneumothorax by radiography and ultrasonography: a meta-analysis. Chest. 2011 Oct;140(4):859-866.
Wilkerson RG et al. Sensitivity of Bedside Ultrasound and Supine Anteroposterior Chest Radiographs for the Identification of Pneumothorax After Blunt Trauma. Acad Emerg Med. 2010 Jan;17(1):11-7.
Skulec R, Parizek T, David M, Matousek V, Cerny V. Lung Point Sign in Ultrasound Diagnostics of Pneumothorax: Imitations and Variants. Emerg Med Int. 2021;2021:6897946.
Steenvoorden TS, Hilderink B, Elbers PWG, Tuinman PR. Lung point in the absence of pneumothorax. Intensive Care Med. 2018;44(8):1329-1330.
Pasternac K, Vermeulen M. Special Commentary: The Bigger Picture: Beware of the Pseudo-Lung Point. ACEP Emergency Ultrasound. 2020 Mar. https://www.acep.org/how-we-serve/sections/emergency-ultrasound/news/march-2020/special-commentarythe-bigger-picture-beware-of-the-pseudo-lung-point/. Accessed 25 Jul 2021.
Gillman LM, Alkadi A, Kirkpatrick AW. The “pseudo-lung point” sign: all focal respiratory coupled alternating pleural patterns are not diagnostic of a pneumothorax. J Trauma. 2009 Sep;67(3):672-3.
Aziz SG, Patel BB, Ie SR, Rubio ER. The Lung Point Sign, not Pathognomonic of a Pneumothorax. Ultrasound Q. 2016 Sep;32(3):277-9.
Zhang Z, Chen L. A physiological sign that mimics lung point in critical care ultrasonography. Crit Care. 2015 Mar 30;19(1):155.