Sternoclavicular Joint Dislocation
Written by Jeremy Riekena, MD
Edited by Victor Huang, MD, CAQ-SM
Figure 1: Posterior sternoclavicular dislocation (https://surgeryreference.aofoundation.org/orthopedic-trauma/adult-trauma/clavicle/medial-extraarticular/reduction-of-sternoclavicular-dislocation)
Introduction
The sternoclavicular joint is the only true point of articulation between the upper extremities and axial skeleton. This articulation is limited to the sterno-clavicular and costo-clavicular surfaces. Nevertheless, this saddle-type joint has inherent stability that is achieved by its four ligamentous attachments [1].
This is a rare injury, making up <1% of all dislocations and 3% of shoulder girdle injuries. High forces are required to destabilize this joint from severe mechanisms such as motor vehicle collisions or sports injuries [2].
Figure 2: Anatomy of the sternoclavicular joint (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2386312/)
Classification and Mechanism of Injury
Injuries to the joint include simple sprains (grade I), subluxations (grade II), and dislocations (grade III) [2]. These occur through direct chest trauma or lateral compression while the arm is held in abduction. Anterior sternoclavicular (SC) joint dislocations are the most common type and can be caused by lateral compression to the anterolateral shoulder with force transmitted medially (image B) [2]. Posterior SC dislocations comprise the other 10% of presentations [3]. This may occur from a direct anterior-to-posterior force applied to the medial clavicle or from posterolateral compression of the shoulder with force transmitted medially (image A). This injury pattern is a true orthopedic emergency with risk for serious injury to the subclavian vasculature, trachea, esophagus, and brachial plexus. 30% of posterior dislocations may have a life threatening complication [2] and carries a 3-4% mortality rate [3].
Figure 3: Mechanism of injury resulting in posterior (left image) and anterior sternoclavicular dislocations (right image) (https://musculoskeletalkey.com/sternoclavicular-injuries/)
Presentation
Patients most commonly present after a traumatic event, but they may on occasion present atraumatically after subluxation from overhead arm elevation. Common complaints include chest, shoulder, and arm pain. Depending on the surrounding structures that may be injured, there may be neurologic, vascular, or aerodigestive symptoms associated. Patients will often be sitting still and upright as pain is typically exacerbated with arm movement and supine positioning [4].
The shoulder may appear more anterior and shortened. The joint itself will demonstrate localized swelling with tenderness, and pain is worsened with glenohumeral or scapulothoracic movement. Their head may be turned toward the affected side as it relieves pressure on the joint [5]. A careful examination of the sternoclavicular joint may aid in delineation of the direction of injury. An anterior dislocation will demonstrate a prominent and anteriorly oriented medial clavicle, while the medial clavicle will be less visible or prominent in posterior dislocations [2]. Be cautious during evaluation as posterior dislocations are more subtle and may be missed without a high index of suspicion. This physical exam may be obscured with delayed presentations, making imaging more important in aiding the diagnosis [6].
Figure 4: Anterior sternoclavicular dislocation (https://www.orthobullets.com/trauma/1009/sternoclavicular-dislocation)
Imaging
X-Ray
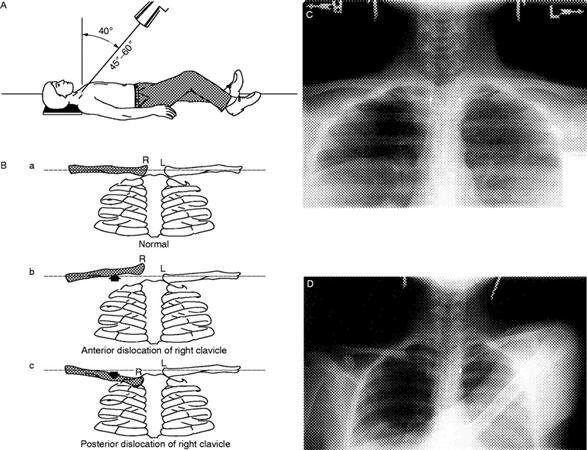
Initial imaging may include a unique view called the serendipity view, which is taken with a 40 degree cephalic tilt [4]. This view is advantageous as standard chest x-rays may obscure evaluation due to overlying bony structures and soft tissues. An AP chest x-ray is useful, however, to evaluate for associated hemo- or pneumothorax. Alternative views include Hobbs and Heinig views.
X-ray findings may demonstrate joint space widening at the sternoclavicular joint. Anterior dislocations show the affected clavicle above the contralateral clavicle. Posterior dislocations show the affected clavicle below the contralateral clavicle.
The physis fuses completely by the age 22-25, which must be considered when evaluating the joint in youth presentations [1].
Figure 5: Serendipity view of sternoclavicular joint dislocation (https://www.orthobullets.com/trauma/1009/sternoclavicular-dislocation)
CT Scan
The gold standard imaging modality is CT scan to demonstrate the relative position of the sternum and clavicle and associated injuries to surrounding structures more clearly [7]. CT scan with angiography further has the advantage of identifying vascular injuries in posterior dislocations [5].
Figure 6: Axial CT image posterior sternoclavicular dislocation (https://radiopaedia.org/articles/sternoclavicular-joint-dislocation?lang=us)
Management
Anterior Dislocation
These injuries are not associated with significant morbidity, so patients can be discharged with nonoperative management. Grade I and II injuries can be treated with analgesia, rest, immobilization with a sling or figure-of-eight splint and routine outpatient Orthopedic follow-up [2,5].
Meanwhile, an anterior dislocation (grade III) should be manually reduced with appropriate analgesia [5]. Closed reduction may be performed within 7-10 days in the Emergency Department or operating room.
The patient is positioned in the supine position with a towel roll in between their scapulae. The affected arm is abducted to 90 degrees and extended to 15 degrees, and inline traction is applied. Additionally, a provider may need to place anterior-to-posterior pressure on the medial clavicle [2,6].
Reduced joints should be stabilized with clavicular splinting with a figure-of-eight brace, sling support, or a velpeau bandage [5,6]. Appropriate follow-up should be made with Orthopedics within several days and return precautions given as 50% may re-dislocate. Most patients will have resolution of pain in 2-3 weeks with return to full physical activity by 3 months [3,5].
Figure 7: Reduction technique for anterior sternoclavicular dislocation (Daya RM, and Bengtzen RR. Shoulder. Rosen’s Emergency Medicine: Concepts and Clinical Practice, 8th ed. Philadelphia, PA: Saunders Elsevier, 2014. pp. 618-642.)
Posterior Dislocation
Indications for emergent closed reduction of posterior dislocations in the ED include airway obstruction, stridor, labored breathing, dysphagia, and neurovascular compromise [2,6].
When the patient is stabilized, Orthopedic surgery should be consulted for closed reduction in the OR. Thoracic and/or vascular surgery should be consulted as well because reduction may damage the great vessels and surrounding neurovascular or aerodigestive structures [5].
There are several reduction techniques to consider:
Classic: the affected arm is abducted and extended with inline traction and anterior traction is applied to the medial clavicle [2].
Towel Clip: if the classic technique is not successful, the skin over the clavicle should prepared under sterile condition. Using a metal towel clip, the medial clavicle is grasped percutaneously and placed under anterolateral traction [2,6].
Buckerfield and Castle: The ipsilateral arm is adducted with caudal traction while an assistant places posterior pressure to the bilateral shoulders [3].
All posterior sternoclavicular dislocations should be admitted for OR management and considered for observation for subsequent injuries because vascular injuries have been reported after reduction [7].
Figure 8: Towel clip reduction technique for posterior sternoclavicular dislocation, (https://surgeryreference.aofoundation.org/orthopedic-trauma/adult-trauma/clavicle/medial-extraarticular/reduction-of-sternoclavicular-dislocation)
References
Roepke C, Kleiner M, Jhun P, Bright A, Herbert M. Chest Pain Bounce-Back: Posterior Sternoclavicular Dislocation. Ann Emerg Med. 2015;66(5):559-561.
Daya RM, and Bengtzen RR. Shoulder. In Marx J.A., Hockberger R.S., and Walls R.M. (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, 8th ed. Philadelphia, PA: Saunders Elsevier, 2014. pp. 618-642.
Sewell MD et al. Instability of the sternoclavicular joint: current concepts in classification, treatment, and outcomes. Bone Joint J 2013; 95-B: 721-31. PMID: 23723264
Balcik BJ et al. Evaluation and treatment of sternoclavicular, clavicular, and acromioclavicular injuries. Prim Care Clin Office Pract 40 (2013): 911-923. PMID: 24209725
Kiel J, Ponnarasu S, Kaiser K. Sternoclavicular Joint Injury. [Updated 2020 Sep 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507894/
Burg MD. Sternoclavicular Joint Dislocation Reduction. Emergency Medicine Procedures. 3rd ed. New York, NY: McGraw Hill; 2019: 864-870.
Deren ME et al. Posterior sternoclavicular dislocations: a brief review and technique for closed management of a rare but serious injury. Orthopedic Reviews 2014; 6: 5245. PMID: 24744842