Ortho/Trauma Case: Jumper - Fall from Height
Author: Ashraf Hussain, MD
Peer-reviewer and Editor: Victor Huang, MD, CAQ-SM
Case: 40-year-old-male with a history of schizophrenia, bipolar disorder and multiple suicide attempts was brought in by EMS as a trauma notification for a suicide attempt after jumping off a two story building. Vital signs are notable for tachycardia, primary survey is intact, and secondary survey demonstrates swelling, ecchymosis and tenderness to the right heel. Neurovascular examination is intact.
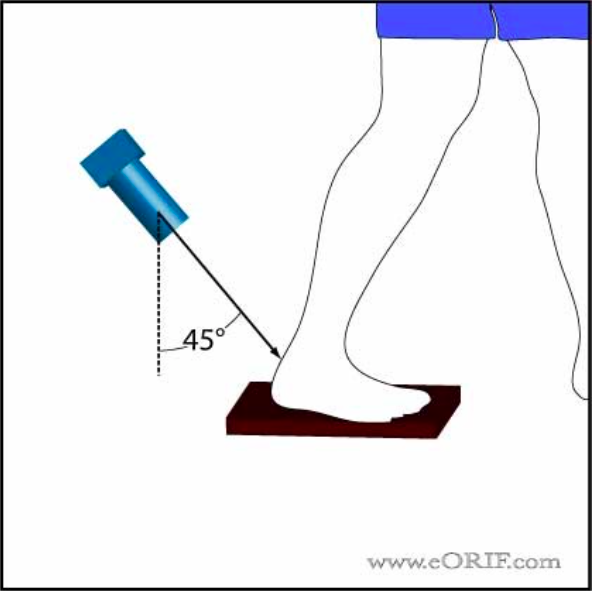
Figure 1: Image Prompt. Plain radiograph lateral view of the right foot. Author’s own images.
What is the diagnosis?
*Comminuted fracture of the calcaneus*
Pearl: The calcaneus is the most commonly fractured tarsal bone [1]. It is associated with a high degree of morbidity if not adequately diagnosed and treated. Overall, it makes up 2% of all fractures. Approximately 75% are intra-articular fractures. Males have more than double the incidence of calcaneal fractures than females [2].
Anatomy
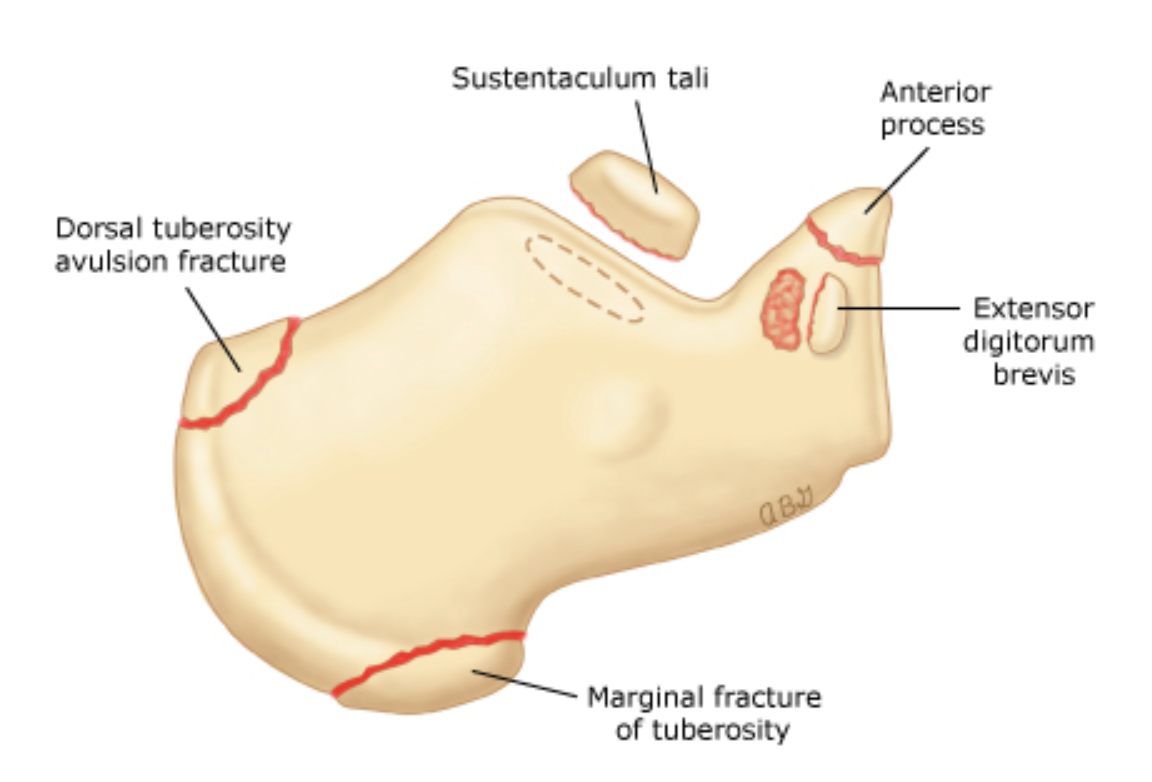
Figure 2: Anatomy of the foot.
What is the mechanism of injury?
Falls from height are the most common mechanism due to increased axial load [3]. Motor vehicle accidents can also cause fractures when the pedal causes impact on the foot. Stress fractures can also occur from overuse, such as with runners. Geriatric patients do not necessarily require high impact injuries due to osteoporosis and osteopenia [4].
What physical exam findings are expected?
The patient will present with severe heel pain, many times unable to bear weight. The heel may appear deformed with shortening. There will be tenderness and swelling around the heel. Ecchymosis may extend from around the heel to the arch of the foot. The skin surrounding the heel should be examined carefully for any breaks or tenting [5].
What modalities can we use to diagnose the fracture?
When suspecting a calcaneus fracture obtain AP, lateral, and oblique plain films of the foot. A Harris view is a specialized view that allows for isolated images of the calcaneus. Obtain CT imaging if there is high clinical suspicion despite negative x-rays. With the lateral x-ray you can measure Bohler’s angle. A decreased Bohler’s angle may indicate a subtle calcaneal fracture. The Bohler's angle is formed by drawing a line from the highest part of the anterior process and the highest part of the posterior articular surface and a line by the same point on the posterior articular surface and the most superior point of the tuberosity. A normal Bohler's angle is between 20-40 degrees. Less than 20 degrees is pathologic [6].
Figure 3: (A) Bohler’s angle; (B) Harris view
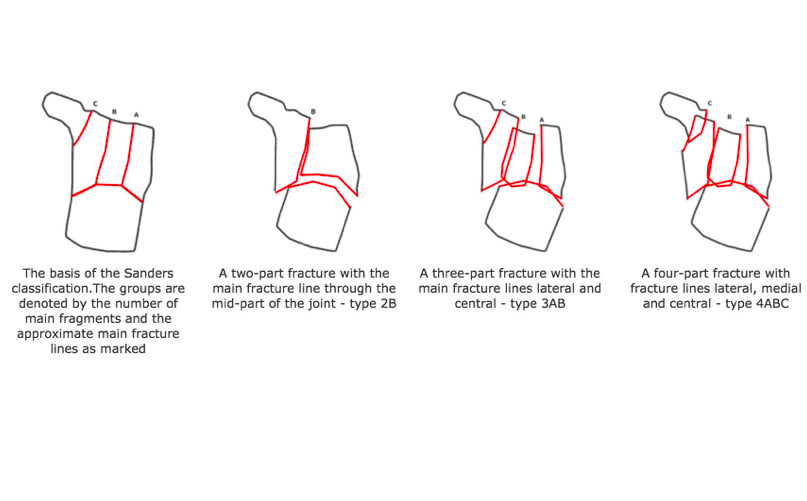
How do we classify the fracture?
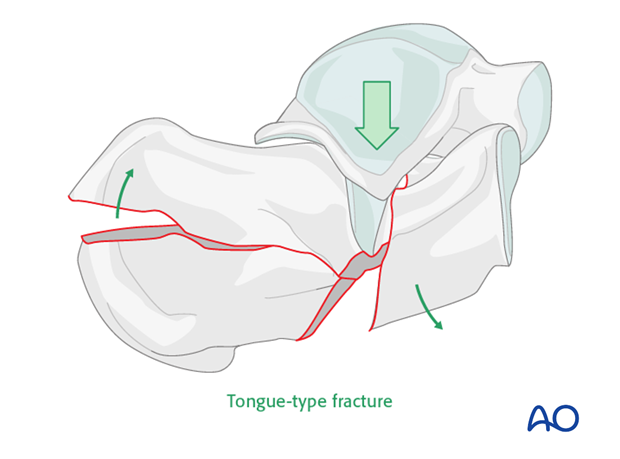
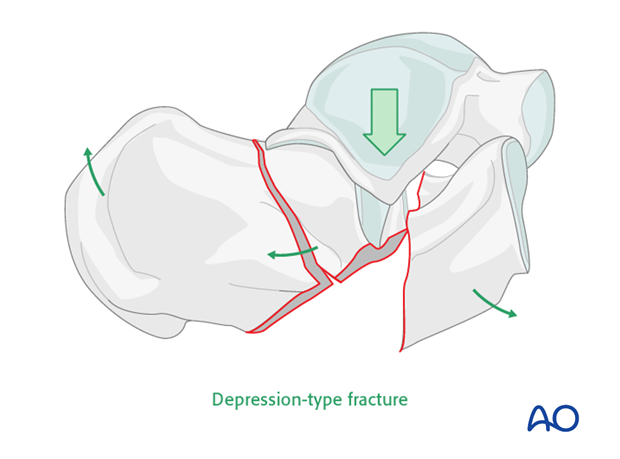
Extra-articular fractures are most commonly avulsion fractures [7]. Intraarticular fractures can be classified using two classification systems. The Essex-Lopresti classification is based upon plain x-rays. The fractures are classified as depression type fractures, or tongue type fractures which exits the calcaneal tuberosity posteriorly. The Sanders classification system is based on CT imagining and has a greater prognostication factor. It is based on the number of articular fragments seen on CT imaging.
Figure 4: (A) extra-articular fractures; (B and C) Essex-Lopresti classification system of intra-articular fractures; (D) Sanders classification of intra-articular fractures.
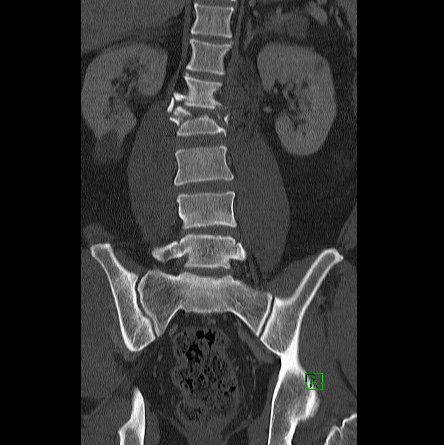
What associated injuries should you look out for?
Vertebral burst fractures can occur with high energy mechanism calcaneal fractures. A recent study demonstrated 7% association [8]. There may be a concurrent achilles tendon injury [5]. There is also up to a 20% association with contralateral calcaneal injury [9].
Figure 5: CT images of the lumbar spine that demonstrate an acute vertebral burst fracture of L2. Author’s own images.
What is the management in the ED?
As the patient will likely be in tremendous pain, be sure to have proper pain control so that you can have a thorough examination of the foot. Frequent neurovascular exams should be performed as 10% of patients may develop compartment syndrome especially in displaced fractures[10,11]. Emergent Orthopedic consultation should be obtained for any open fracture, displaced extra-articular fracture, any fracture greater than Sanders type 1 or tongue type fracture, dislocation/fracture, or neurovascular injury. All other fractures can be placed in a posterior leg splint, made non-weight bearing and follow-up with Orthopedics [3,5].
Works Cited
Eiff MP, Hatch RL. Fracture Management for Primary Care, 3rd, Elsevier Saunders, Philadelphia 2012.
Mitchell MJ, McKinley JC, Robinson CM. The epidemiology of calcaneal fractures. Foot (Edinb). 2009 Dec;19(4):197-200. doi: 10.1016/j.foot.2009.05.001. PMID: 20307476.
Sanders RW, Clare MP. Calcaneus fractures. In: Rockwood and Green's Fractures in Adults, 7th, Bucholz, RW, Heckman JD, Court-Brown CM, Tornetta P (Eds), Lippincott Williams & Wilkins, Philadelphia 2010. p.2064.
Rupprecht M, Pogoda P, Barvencik F, et al. The calcaneus as the site of manifestation for osteoporosis-associated fractures: age- and sex-specific changes in calcaneal morphology correlate with the incidence and severity of intra-articular calcaneal fractures. Unfallchirurg. 2007;110(3):197-204. doi:10.1007/s00113-006-1187-1.
Davis D, Seaman TJ, Newton EJ. Calcaneus Fractures. In: StatPearls. Treasure Island (FL): StatPearls Publishing; August 8, 2020.
Loucks C, Buckley R. Bohlers Angle: Correlation With Outcome in Displaced Intra-articular Calcaneal Fractures. Journal of Orthopaedic Trauma. 1999;13(8):554-558. doi:10.1097/00005131-199911000-00007
Schweitzer ME, Karasic D. The Foot. In: Radiology of Skeletal Trauma, 3rd, Rogers LF (Ed), Churchill Livingstone, Philadelphia 2002. p. 1319.
Walters JL, Gangopadhyay P, Malay DS. Association of Calcaneal and Spinal Fractures. The Journal of Foot and Ankle Surgery. 2014;53(3):279-281. doi:10.1053/j.jfas.2014.01.012
Leite CBG, Macedo RS, Saito GH, Sakaki MH, Kojima KE, Fernandes TD. Epidemiological study on calcaneus fractures in a tertiary hospital. Rev Bras Ortop. 2018;53(4):472-476. Published 2018 Jun 13. doi:10.1016/j.rboe.2018.05.014
Baumhauer JF, Manoli A 2nd. Principles of management of the severely traumatized foot and ankle. Instr Course Lect. 2002;51:159-67. PMID: 12064101.
Germann CA, Perron AD, Miller MD, Powell SM, Brady WJ. Orthopedic pitfalls in the ED: calcaneal fractures. Am J Emerg Med. 2004 Nov;22(7):607-11. doi: 10.1016/j.ajem.2004.09.008. PMID: 15666272.