Time is Testes!
Written by: Dr. John Lin
Edited by: Dr. Joann Hsu
The case:
An 18 year old male with no significant past history presents at 11:30 AM with complaints of acute left testicular pain since this morning. The pain began suddenly at 7:30 AM and radiated to his epigastric area, associated with nausea.
Exam on the patient was only notable for left scrotal tenderness, edema, and high-riding testes. Cremasteric reflex was intact.
Acute testicular torsion was suspected; however given intact cremasteric reflexes further studies were obtained.
Bedside ultrasound was concerning for lack of blood flow to the left testicle, and urology was immediately consulted
Radology-performed ultrasound was obtained emergently (see Figure 7) which confirmed loss of blood flow to the left testes, indicating testicular torsion.
BACKGROUND:
Figure 1: Normal testicular anatomy versus testicle with abnormal tunica vaginalis (bell clapper deformity.1
Testicular torsion is a medical emergency that presents as a sudden, intermittent and severe scrotal pain, often accompanied by nausea and vomiting.
The pain is typically localized to the affected testicle and may be associated with swelling and erythema.
The affected testicle may be positioned abnormally compared to the unaffected side (horizontal lie, however position is variable), and may be tender and hard on palpation.
The cremasteric reflex may be assessed: by stroking the inner thigh gently, the cremaster muscle pulls the testicle closer to the body and elevates the testes.
This reflex may be absent in torsion but it is no longer a sensitive or specific test since it may also not be present in some healthy adults and adolescents.
The pathophysiology of testicular torsion involves the rotation of the testicle causing twisting of the vascular bundle in the spermatic cord, leading to ischemia and subsequent necrosis of the testicular tissue.
The age range of men affected by torsion varies with two peak incidences, one during neonatal period and second and largely during adolescence between ages 12-18. (1)
Congenital anatomic abnormalities, such as the bell-clapper’s deformity, can increase the risk of testicular torsion in infants.
This is because the tunica vaginalis, which normally secures the testicle in place, fails to do so, allowing for unrestricted rotation of the testicle.
Other risks, such as trauma to the testes can also lead to torsion.
ULTRASOUND:
Ultrasound findings of testicular torsion may include a high-riding testicle on ultrasound, with absent or decreased blood flow on doppler imaging.
The diagnostic ultrasound only has a sensitivity of 76% (4) patients may have torsion-detorsion, so seeing blood flow does not rule out definitive torsion.
However, seeing lack of flow on ultrasound is highly suggestive of active torsion.
Below is a brief overview of normal testicular ultrasound and findings of testicular torsion.
Normal ultrasound of the testes includes the following views: buddy view, each testes in transverse and sagittal views with and without color, and epididymis. Use the linear ultrasound probe to assess.
Buddy View:
Place the linear probe in transverse over both testes. May use the patient’s inner thigh muscle or towel to support the testes inferiorly.
Fan through the testes to assess for any obvious asymmetry - ischemic testicles become heterogeneous in appearance and edematous.
Place color to assess for general vascular flow. Use the unaffected testes to calibrate the intensity of color and then assess side-by-side with the affected testes (Figure 3)
Power doppler can be used to measure a resistance index (RI). RI = (peak systolic velocity - end diastolic velocity) / peak systolic velocity.
Higher RI implies diminished diastolic flow through the vascular bed, often due to poor venous outflow and venous congestion in the setting of torsion.
After a detorsion event, the edema may limit diastolic flow and RI may remain elevated.
A normal resistive index is less than 0.7 and higher values indicative high vascular resistance in the testes (Figure 4)
Figure 3 - Buddy view showing normal color flow with similar intensity in bilateral testes
Figure 4 - Measurement of Resistive Index (RI) in the unaffected testicle.
Transverse and Sagittal View:
Focusing on each testes, obtain transverse and sagittal measurements by fanning in the long and short plane and then measure a volume
May also assess for color in each of these views to further confirm whether there is vascular flow
Figure 5a: transverse (short) view of normal testicle
Figure 5b: Longitudinal view of normal testicle
Epididymis view:
The epididymal head is located in the superior and posterior aspect of the testicle. It is best viewed in the sagittal plane or long axis. It often appears triangular with a normal measurement of 1 cm in height and 1cm at the base.
Figure 6 - left epididymal head
In testicular torsion, there are multiple findings on ultrasound that can help make the diagnosis.
In the buddy view, there will be a lack of color flow in the affected testes during active torsion.
Additionally in torsion-detorsion where one does see color on the buddy view, the resistive index may still be abnormally elevated.
Surrounding the affected testes, there may be a reactive hydrocele that develops and the size of the testes may be noticeably larger (normal volume of testes ~ 3 x 4 x 5 cm).
Finally, during active torsion, one may see the whirlpool sign where the spermatic cords are actively twisted in the scrotum.
Figure 7: Buddy View with lack of testicular blood flow over left testes (right image)
Figure 8 - Reactive hydrocele in left testes with confirmed torsion
Figure 9: High Resistive Index after detorsion, likely underestimated.
Figure 10 - Whirlpool sign, spermatic cord twisting (5)
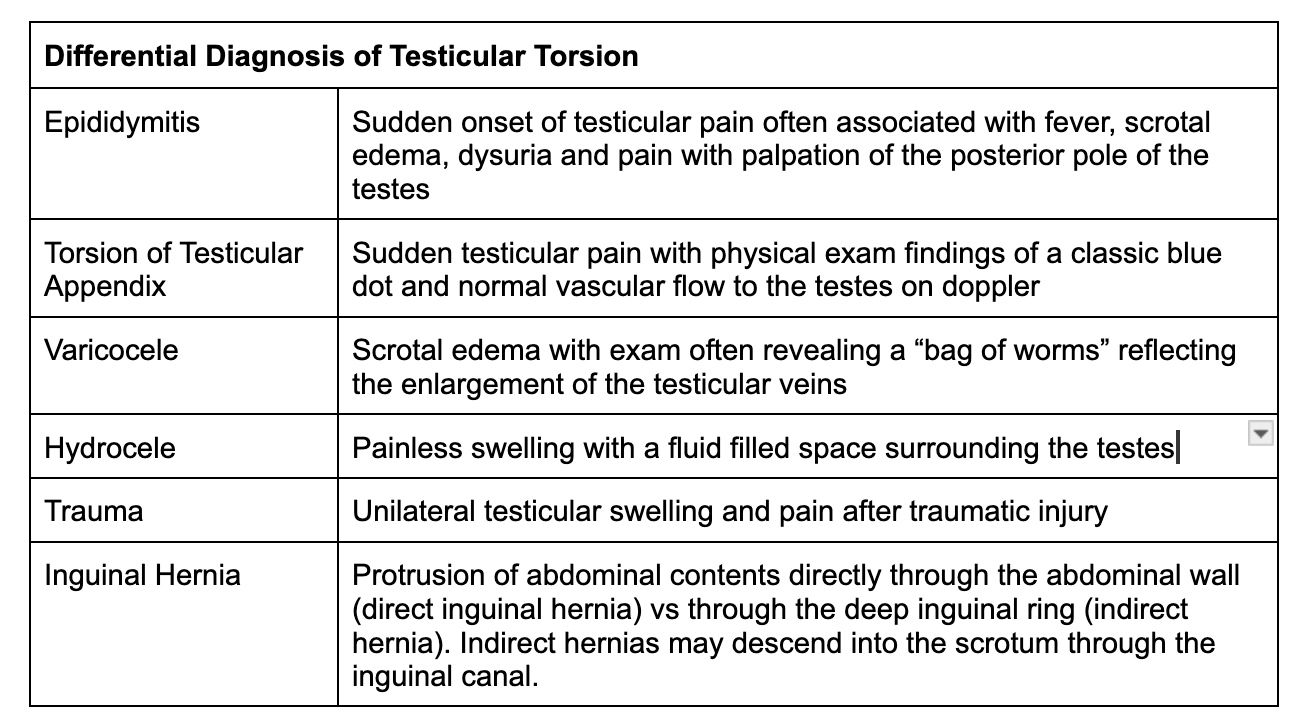
The diagnosis of testicular torsion is made based on clinical presentation and confirmed with imaging studies. It is important to differentiate testicular torsion from other causes of scrotal pain, such as epididymitis or torsion of the appendix testis (see full list of differentials).
Management of testicular torsion involves emergent surgical intervention to restore blood flow to the affected testicle.
In the emergency room, confirmed torsion especially if visualizing the lack of blood flow on ultrasound, the open book method may be attempted: rotate the affected testes medial to lateral 540 degrees. (3)
Pain should improve and vascular flow will return after detorsion (see below). If pain worsens during manual detorsion, rotate the testes the other way.
Figure 11: open book method employing a 360-540 rotation laterally to untwist the spermatic cord4
Figure 12: post manual detorsion in the emergency using the open book method. Left testes with return of vascular flow, compare with Figure 7 (same testes)
Confirmed or highly suspected torsion requires an emergent urologic consult.
Successful detorsion still should get a urological evaluation or orchiopexy to prevent future torsion. In cases where the testicle has undergone irreversible damage, or if diagnosis and surgical intervention are delayed, orchiectomy (surgical removal of the testicle) may be necessary to prevent further complications.
Delay in diagnosis and treatment can lead to loss of the affected testicle and potential infertility.
In cases where testicular torsion is suspected, it is critical to consult a urologist or other experienced surgeon immediately for prompt evaluation and management.
Case resolution:
On immediate visualization of ischemia to the left testes, the open-book method was applied and the patient reported improvement of pain after 360 lateral rotation.
Reapplying the probe over the left testes demonstrated return of flow (Figure 12).
Urology was updated after official ultrasound findings.
Patient was scheduled for surgical orchiopexy.
References
Causes of scrotal pain in children and adolescents, last updated Aug 2022 (https://www.uptodate.com/contents/causes-of-scrotal-pain-in-children-and-adolescents?search=testicular%20torsion&source=search_result&selectedTitle=2~40&usage_type=default&display_rank=2)
Testicular Torsion, revised by Ciro Mauro on 7 Feb 2023, https://radiopaedia.org/articles/testicular-torsion?lang=us
https://wikem.org/wiki/Testicular_torsion
https://radiopaedia.org/articles/whirlpool-sign-testicular-torsion?lang=us