Is it Tamponade
Written by: Dr. David Poloway
Edited by: Dr. Joann Hsu
The case:
51-year-old female with a history of Lupus and fibromyalgia, who presents with complaints of shortness of breath. Patient has been having upper respiratory symptoms with runny nose, cough, chills with no fever x few days. Patient reports having shortness of breath today along with nausea and non-bloody, non-bilious vomiting over the last evening. No chest pain or leg swelling.
BP: 118/84 // HR: 111 // SpO2: 95% on 2L N
Physical exam significant for tachypnea
In the setting of shortness of breath, you decide to take your ultrasound and do a bedside echo and lung ultrasound.
Here is this patient’s parasternal long view:
What is tamponade?
First of all, an effusion must be present. However, tamponade physiology may be present with a small effusion or very large one.
The pericardium is a fibroelastic sac which may stretch. The rate of fluid accumulation is what ultimately determines if tamponade physiology will be present. With slow accumulation, the pericardium has time to slowly stretch. However, with rapid accumulation, the pericardium has little time to stretch and normally this results in tamponade.
So how do we diagnose this? Remember in medical school when we were taught Beck’s Triad? Well, as it turns out, hypotension, jugular venous distension, and muffled heart sounds are incredibly non-specific and inaccurate, and are all commonly very late findings. [kapoor]
The primary physiological disturbance is due to compression of the cardiac chambers secondary to increased pressure in the pericardium (from an effusion) which exceeds diastolic filling pressures. This leads to impaired filling of the heart. If we think about it this way, it’s easier to understand the ultrasonography signs of tamponade, a cannot miss emergency medicine diagnosis!
So, to have cardiac tamponade:
Pericardial effusion must be present
Right atrial collapse during ventricular systole (atrial diastole)
MV and TV will be CLOSED
Right ventricular collapse during ventricular diastole (most specific finding) - this is what you look for on ultrasound since right atrial collapse during systole may be hard to visualize
MV and TV will be OPEN
Collapse of a chamber which should be filling!
Plethoric IVC (most sensitive finding) - Indicative of elevated right sided filling pressures
So what do you look for on ultrasound?
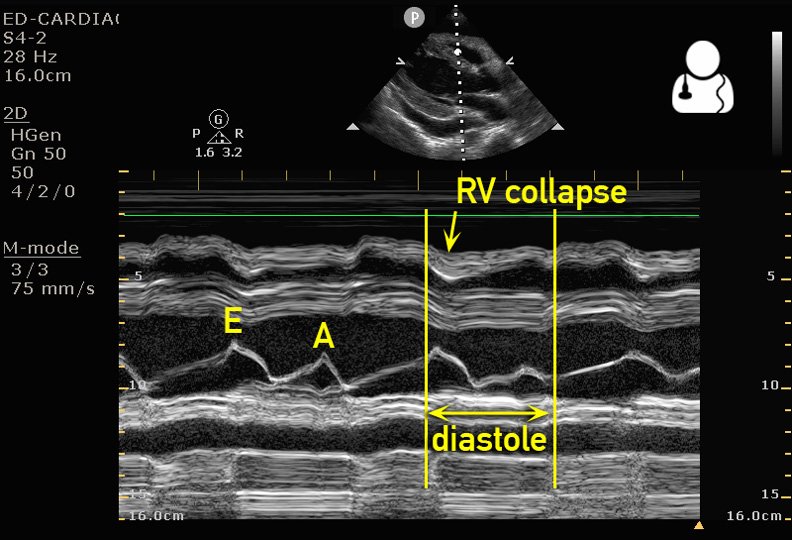
Most simply: Look for RV collapse when the MV is open (diastole). Usually in PSL but can also be seen in your A4 view.
A more objective measure of this is using M mode:
To use M mode, obtain your PSL view.
In this view, the anterior leaflet of the mitral valve should be clearly seen along with the free wall of the right ventricle.
By using M-mode we can record, in real time, the movement of both the mitral valve and the free wall of the right ventricle.
If the wall of the right ventricle collapses when the mitral valve is open (diastole), then RV collapse during diastole is present and we can say that tamponade physiology is present. See attached image below.
It is important to note: tamponade physiology on ultrasound (sonographic evidence of tamponade) may NOT always equate to actual hemodynamic instability. It is very important to recognize tamponade physiology in every pericardial effusion you see so you may call your consultants in a timely manner.
Here is another nice source on tamponade physiology:
https://www.aliem.com/differentiating-pericardial-effusion-tamponade-ultrasound/