Ortho Case: A Fall Down Stairs Wasn't Very Humerus
Author: Nathalie Briones, MD
Peer-reviewer and Editor: Victor Huang, MD, CAQ-SM
Case: 30 year old male, right hand dominant, presenting to the ED with left elbow pain and swelling after a mechanical fall down 5 steps. He denies any head or neck injury, loss of consciousness, or numbness/weakness of the affected extremity. Vital signs are stable. Examination shows gross elbow deformity with prominence of the posterior aspect of the elbow. He is neurovascularly intact distal to the site of injury.
Figure 1. Plain radiographs, AP views of the left elbow and left humerus. Author’s own images.
What is the diagnosis?
What are the mechanisms of injury?
What physical exam findings are expected?
Which imaging modalities can be used?
What is the management in the ED?
What is the definitive management of this injury?
See below for answers!
What is the diagnosis?
The image shows a significantly displaced extra-axial distal humerus fracture, type A2 (AO/OTA classification).
PEARL: Multiple classification systems have been developed to describe distal humerus fractures, however, the AO/OTA classification is the most commonly used internationally [1], which describes the fractures as either extra-articular (Type A), partial articular (Type B), and complete articular (Type C), each with subtypes based on the specific fracture pattern and degree of comminution [2,3].
Figure 2. AO/OTA classification of distal humerus fractures (From Journal of orthopaedics trauma. Marshet al. 2007) [4].
What are the mechanisms of injury?
Distal humerus fractures can be caused by direct impact to the elbow, or indirect impact after a fall on an outstretched hand. These fractures have a bimodal distribution in adults. Although classically seen following high-energy trauma in young males, there has been an increasing incidence amongst elderly females following low energy trauma [1-4].
What physical exam findings are expected?
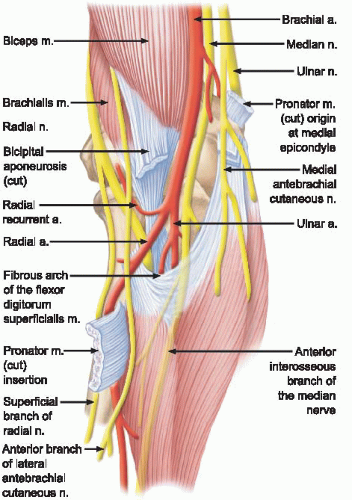
The patient is likely to present with pain and swelling to the elbow. The physical examination should include a thorough neurovascular exam, documenting distal pulses and radial, PIN, median, AIN, and ulnar nerve function [3,5]. Gross instability is often present with these fractures, therefore avoid ranging the elbow due to the risk of neurovascular injury [3].
PEARL: Injury to the brachial artery is possible due to its anatomic proximity over the anterior-medial aspect of the elbow. The radial nerve is the most commonly injured. Examination of the forearm compartments should be performed to assess for acute compartment syndrome [3,5].
Which imaging modalities can be used?
Plain radiographs of the elbow and humerus including AP and lateral views should be obtained. Traction views may also be helpful to remove bone overlap and evaluate for intra-articular extension. Additional radiographs (e.g. forearm) may also be obtained if other sites of tenderness or injuries are noted on physical examination. CT imaging is useful for surgical planning [3,5].
Figure 4. Computed tomography of the left distal humerus fracture. Author’s own images.
What is the management in the ED?
The injury should be managed with appropriate analgesia and closed reduction and immobilization in a posterior long-arm splint with the elbow flexed to 90 degrees and the forearm in neutral position. Post-reduction neurovascular exam and imaging should be performed. Orthopedics should be consulted emergently for open fracture, neurovascular compromise, and acute compartment syndrome [5].
What is the definitive management of this injury?
Surgical management is indicated in the majority of cases, with non-operative treatment reserved only for select cases including non-displaced fractures and patients who are high-risk surgical candidates [1-5].
In most patients, open reduction and internal fixation with contoured locking plates have successful patient outcomes and can achieve pre-injury levels of functional status [4]. However, in cases not amenable to ORIF (e.g. bicolumnar fractures in elderly patients, significant comminution and intraarticular involvement), total elbow arthroplasty and elbow hemiarthroplasty are considered good alternatives [1-4].
Case Resolution
In the case discussed above, the patient was managed in the ED with appropriate analgesia and a bedside closed reduction with traction-countertraction. He was placed in a well-padded posterior long-arm splint with side slabs. Repeat neurovascular examination was normal and post-reduction plain films and CT imaging were performed. He was kept non-weight bearing in a sling at all times. He followed up with Orthopedics in 1 week, and underwent ORIF.
Works Cited
Amir S, Jannis S, Daniel R. Distal humerus fractures: a review of current therapy concepts. Curr Rev Musculoskelet Med. 2016;9(2):199-206. doi:10.1007/s12178-016-9341-z
Anglen J. Distal humerus fractures. J Am Acad Orthop Surg. 2005;13(5):291-297. doi:10.5435/00124635-200509000-00001
Crean TE, Nallamothu SV. Distal Humerus Fractures. [Updated 2020 Jul 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK531474/
Ul Islam S, Glover AW, Waseem M. Challenges and Solutions in Management of Distal Humerus Fractures. Open Orthop J. 2017;11(1):1292-1307. doi:10.2174/1874325001711011292
Eiff MP, Hatch R. Elbow Fractures. In: Fracture Management for Primary Care. 3rd Ed. Elsevier; 2018:141-147



![Figure 2. AO/OTA classification of distal humerus fractures (From Journal of orthopaedics trauma. Marshet al. 2007) [4].](https://images.squarespace-cdn.com/content/v1/5bc94f5b9b7d1515843688af/1612473462719-FQA3N7Q1Z9TZIZ89WAPG/Screen+Shot+2021-01-29+at+11.54.36+AM.png)