Ortho Case: My Arm Is Stuck Like This
Author: William Chan, MD
Peer-reviewer and Editor: Victor Huang, MD, CAQ-SM
Case
A 70-year-old female presents to the emergency room with right shoulder pain, deformity, and decreased range of motion after a trip and fall on the sidewalk. Patient is unable to adduct her arm.
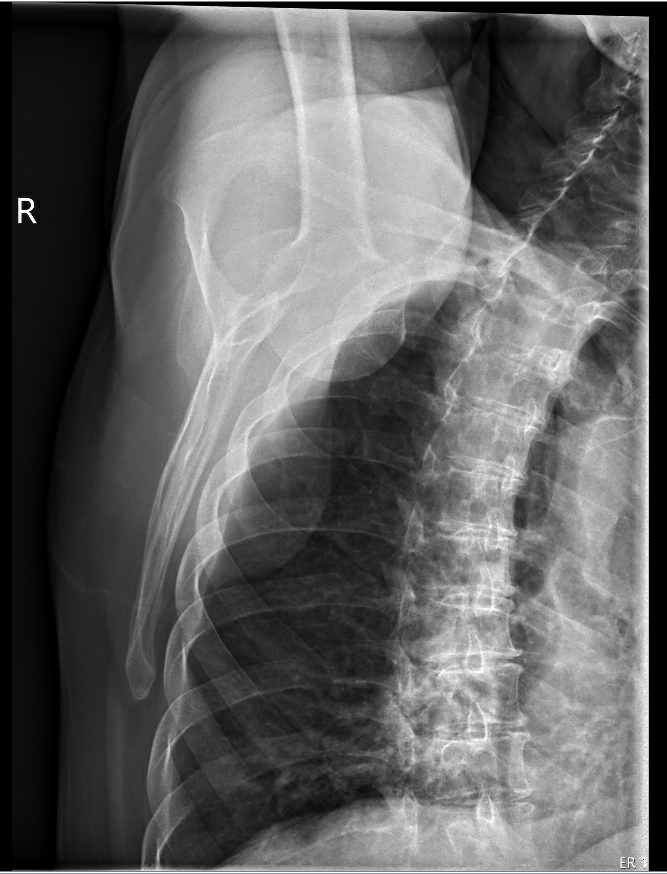
Figure 1. Image Prompt. AP, scapular Y and axillary plain radiograph of the right shoulder. Author’s own images.
Diagnosis
Inferior shoulder dislocation, aka Luxatio Erecta.
General
Shoulder dislocation is one of the most common dislocations seen in the Emergency Department, and represents 50% of all major joint dislocations [1]. In 2017, there were approximately 0.4 million visits for dislocations in the United States [2]. Although anterior dislocations are frequently seen in the emergency room, inferior dislocations, represent only 0.5% of all shoulder dislocations [3].
Mechanism of injury
The two main mechanisms of injury typically require high-energy trauma. First is axial loading through a fully abducted arm which drives the humeral head through the weaker inferior glenohumeral ligaments [4]. The second is a hyperabduction force to the arm which levers the proximal humerus on the acromion and results in injury to the inferior and middle glenohumeral ligaments [4].
Physical Exam
Given the unique clinical presentation of this dislocation, diagnosis can nearly be made from physical exam alone. The arm is typically in a fixed abducted position above the patient’s head with the humeral head palpable in the axilla. Classically, the elbow is flexed and the forearm is pronated [4]. The brachial plexus and axillary artery course in the axilla, inferior to the glenohumeral joint [5]. Have a high index of suspicion of possible distal neurovascular injury as the humeral head disrupts this space in an inferior dislocation.
Imaging
Plain radiographs are used to confirm the diagnosis and look for associated fractures. The humeral head is displaced inferiorly from the glenoid fossa. A distinct radiological feature of inferior dislocations is that the humeral head is typically parallel to the spine of the scapula [4]. Whereas in anterior dislocations, the arm is adducted and the shaft of the humerus is parallel with the chest wall [4]. Further imaging can be performed including CT to evaluate for associated fracture, and MRI to look for rotator cuff tears, labral tears, and joint capsule injury [6].
ED Management
Closed reduction should be performed in the ED. Two methods have been described for this reduction. The first method is traction-countertraction where axial traction is applied in the direction of the abducted humerus and countertraction is provided by a rolled sheet across the top of the shoulder [4, 6]. However, this reduction can be difficult and typically requires procedural sedation [6].
The second method involves rotating the head of the humerus from an inferior position to an anterior position relative to the glenoid [4,6,7]. The patient should be supine and the provider should stand on the affected side next to the head of the patient. One hand should be placed on the lateral aspect of the mid shaft of the humerus and push the humeral head to the anterior position [6,7]. Meanwhile, the other hand should be positioned over the medial epicondyle and provide gentle superior directed force [6,7]. The resulting action converts the inferior dislocation to an anterior dislocation [4,6,7]. From this position a variety of anterior dislocation reduction maneuvers can be performed.
Definitive Management
In most cases, non-operative treatment with sling immobilization for 2-3 weeks followed by physical therapy is appropriate [4]. Operative management may be needed for neurovascular injury, fracture-dislocation, capsular reconstruction, rotator cuff injury, and irreducible dislocations when the humeral head “buttonholes” through the inferior capsule [3,4,7]. One review of 199 patients from 101 articles found that 15 patients (8%) required operative management [4].
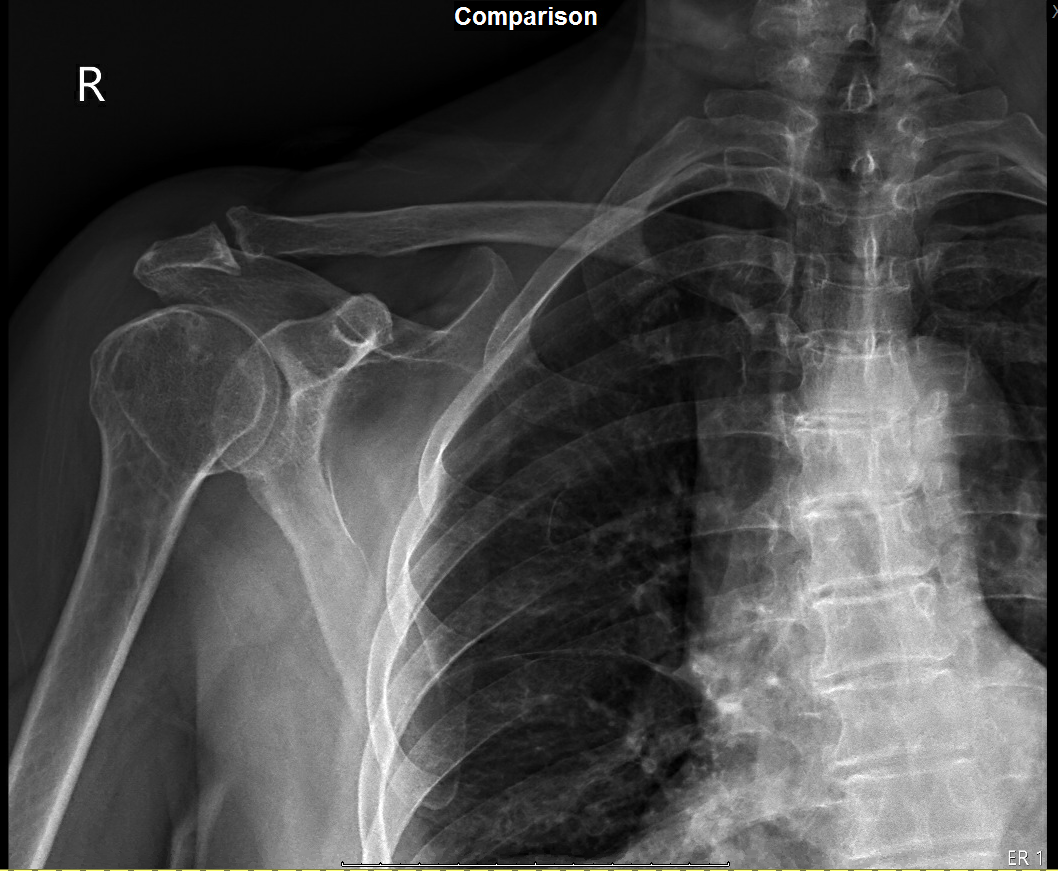
Figure 2. Post-reduction radiographs. Author’s own images.
References
[1] Alkaduhimi H, van der Linde JA, Flipsen M, van Deurzen DF, van den Bekerom MP. A systematic and technical guide on how to reduce a shoulder dislocation. Turk J Emerg Med. 2016 Nov 18;16(4):155-168. doi: 10.1016/j.tjem.2016.09.008. PMID: 27995208; PMCID: PMC5154590.
[2] Rui P, Kang K. National Hospital Ambulatory Medical Care Survey: 2017 emergency department summary tables. National Center for Health Statistics. Available from: https://www.cdc.gov/nchs/data/nhamcs/web_tables/2017_ed_web_tables-508.pdf.
[3] Groh GI, Wirth MA, Rockwood CA Jr. Results of treatment of luxatio erecta (inferior shoulder dislocation). J Shoulder Elbow Surg. 2010 Apr;19(3):423-6. doi: 10.1016/j.jse.2009.07.062. PMID: 19836975.
[4] Nambiar M, Owen D, Moore P, Carr A, Thomas M. Traumatic inferior shoulder dislocation: a review of management and outcome. Eur J Trauma Emerg Surg. 2018 Feb;44(1):45-51. doi: 10.1007/s00068-017-0854-y. Epub 2017 Oct 3. Erratum in: Eur J Trauma Emerg Surg. 2017 Nov 20;: PMID: 28975397.
[5] Orebaugh SL, Williams BA. Brachial plexus anatomy: normal and variant. ScientificWorldJournal. 2009 Apr 28;9:300-12. doi: 10.1100/tsw.2009.39. PMID: 19412559; PMCID: PMC5823154.
[6] Yao F, Zhang L, Jing J. Luxatio erecta humeri with humeral greater tuberosity fracture and axillary nerve injury. Am J Emerg Med. 2018 Oct;36(10):1926.e3-1926.e5. doi: 10.1016/j.ajem.2018.06.064. Epub 2018 Jun 27. PMID: 30238913.
[7] Nho SJ, Dodson CC, Bardzik KF, Brophy RH, Domb BG, MacGillivray JD. The two-step maneuver for closed reduction of inferior glenohumeral dislocation (luxatio erecta to anterior dislocation to reduction). J Orthop Trauma. 2006 May;20(5):354-7. doi: 10.1097/00005131-200605000-00010. PMID: 16766940.