Ortho Case: Elbow Injury
Author: Victor Huang, MD
Case: A 70-year-old female presents to the Emergency Department for left elbow pain and deformity after tripping on an uneven sidewalk and falling on an outstretched hand. She denies any head injury, neck pain, loss of consciousness, or use of blood thinners. She has a history of breast cancer status post mastectomy and lymph node removal with resulting lymphedema. Vital signs are stable. Examination shows gross elbow deformity with a shortened forearm and a prominent olecranon with the elbow held in 45 degrees of flexion. She is neurovascularly intact distal to the site of injury.
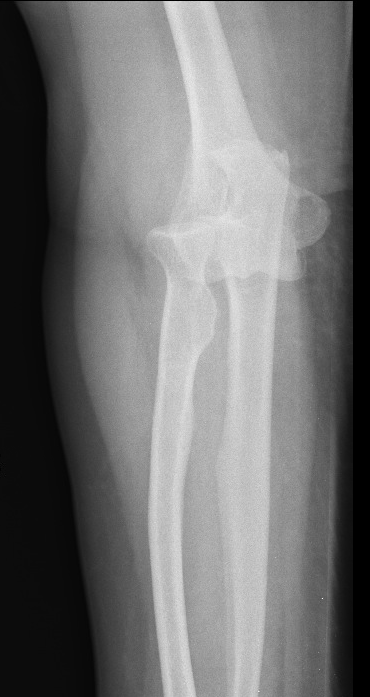
Figure 1: AP and lateral views of the left elbow. Author’s own images.
What is the diagnosis and management in the Emergency Department?
See below for answers!
Diagnosis: Posterior Elbow Dislocation
Case Resolution:
Plain radiography of the left elbow (Figure 1) shows a posterior elbow dislocation with tiny avulsion fractures from the posterior distal humerus.
Propofol 1 mg/kg was utilized for procedural sedation to facilitate the reduction. Traction-countertraction reduction maneuver was used in the supine position. Then, downward pressure was placed on the forearm and anteriorly-directed pressure was placed on the posterior aspect of the olecranon. Reduction elicited a palpable clunk, resolution of elbow deformity, and a return of near-normal range of motion.
Post-reduction x-ray shows a reduced elbow joint. Repeat neurovascular examination was normal and the patient was discharged in a posterior long arm splint. The patient had outpatient Orthopedic management with 2 weeks of immobilization, which was complicated by increased extremity edema. She underwent a progressive rehabilitation program for 12 weeks with OT, PT and lymphedema therapy. She restored her ability to perform ADLs and IADLs but had residual loss of elbow extension of 10 degrees.
Figure 2: Post-reduction radiographs of the left elbow demonstrating a reduced elbow joint. Author’s own images.
Discussion:
Elbow dislocations are the second most common joint dislocation with an annual incidence of 6 to 13 cases per 100,000 people [1-5]. Simple elbow dislocations are characterized by the absence of a major associated fracture, aside from small periarticular avulsion fractures [2,5]. Meanwhile, complex dislocations have a significant fracture of the radial head, olecranon, coronoid, or humeral epicondyles [1-6].
Elbow dislocations are classified by the direction of displacement of the radius and ulna relative to the humerus: posterior, anterior, lateral, medial, and divergent [1-6]. Posterior dislocations, more specifically posterolateral dislocations, are the most common type of elbow dislocations (80%) [1-6]. The typical mechanism of injury for posterior dislocations is a fall resulting in axial loading on an extended elbow combined with a valgus force [1-6]. Anterior dislocations are rare and result from a direct impact onto the posterior aspect of the olecranon of a flexed elbow [1,3,4].
Examination of a posterior dislocation typically has the elbow held in 45 degrees of flexion, with shortening of the forearm, and prominence of the olecranon posteriorly [1,2,4]. Meanwhile, anterior dislocations will have an extended elbow, elongated forearm, and a prominent distal humerus posteriorly [1,4]. A careful neurovascular examination should be performed to assess for brachial artery and median and ulnar nerve injuries[1-6]. Brachial artery disruption is the most serious complication and it occurs in 5 to 13% of cases [1-4].
Plain radiographs should be performed with anteroposterior and lateral views of the elbow to assess the type of dislocation and look for associated fractures [1-6]. Complex elbow dislocations may benefit from computed tomography scanning for surgical planning [2,5].
Management in the ED should include analgesia prior to reduction. An intraarticular injection of local anesthetic may provide adequate analgesia for a perched dislocation, where the coronoid is impinged on the trochlea [1,3,4]. However, the majority of cases should be performed under procedural sedation [1-4].
Reduction of elbow dislocations is achieved with longitudinal traction of the supinated forearm with the elbow flexed at 25 to 30 degrees, with countertraction of the upper arm [1-3]. Any medial or lateral displacement should be corrected during this maneuver [1,2,6]. Posterior dislocations may require additional downward pressure at the proximal forearm and anterior pressure behind the olecranon [1,4]. Meanwhile, anterior dislocations are reduced with traction and backward pressure on the proximal forearm [1,4].
Post-reduction neurovascular examination and radiographs should be performed [1-6]. Assess for stability of the elbow through its normal range of motion and perform varus and valgus stress testing [1-6]. Stable reductions should be immobilized in a posterior splint with 90 degrees of elbow flexion for 3 to 5 days [1-6]. Early active mobilization has shown improved outcomes compared to plaster immobilization, and immobilization for longer than 2 to 3 weeks should be avoided [2,3,5].
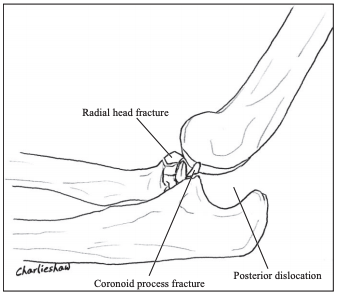
Emergent consultation is required for open dislocations, vascular disruption, and compartment syndrome [1-3]. Orthopedic intervention is indicated for irreducible and chronic dislocations, incarcerated tissue resulting in a locked elbow dislocation, and grossly unstable elbows [2,3,5]. Operative treatment is also recommended for the majority of “terrible triad” cases, which is an elbow dislocation with associated fractures of the radial head and coronoid process, because it can be complicated by recurrent instability and post-traumatic arthrosis [3,6].
Figure 3: AP and lateral views showing the “terrible triad of the elbow,” which is an elbow dislocation associated with radial head/neck fracture and ulnar coronoid process fracture. Courtesy of Dr. Jeremy Jones, rID: 10499.
Works Cited:
Mayer TA. Humerus and Elbow. Rosen’s Emergency Medicine Concepts and Clinical Practice. 8th ed. Philadelphia, PA: Elsevier Saunders; 2014: 612-614.
Grazette AJ, Aquilina A. The Assessment and Management of Simple Elbow Dislocations. The Open Orthopaedics Journal. 2017;11:1373–1379. doi:10.2174/1874325001711011373.
Khan SO, Field LD. Elbow Dislocations in the Adult Athlete and Pediatric Patient. DeLee & Drez’s Orthopaedic Sports Medicine: Principles and Practice. 3rd ed. Philadelphia, PA: Elsevier Saunders; 2009: 1300-1310.
Horn AE, Ufberg JW. Management of Common Dislocations. Roberts & Hedges’ Clinical Procedures in Emergency Medicine. 6th ed. Philadelphia, PA: Elsevier Saunders; 2014: 973-978.
Robinson PM, Griffiths E, Watts AC. Simple Elbow Dislocation. Shoulder & Elbow. 2017;9(3):195–204. doi:10.1177/1758573217694163.
Smith WR, Stahel PF, Suzuki T, Gabrielle P. Musculoskeletal Trauma Surgery. Current Diagnosis & Treatment in Orthopedics, 5th ed. New York, NY: McGraw-Hill; 2014. http://accessmedicine.mhmedical.com/content.aspx?bookid=675§ionid=45451708. Accessed April 06, 2020.