The Threat of Sweat
Written By: Brian Smith, DO
Welcome to another episode of ECG of the Week!
We have a very interesting one to dissect today, so let’s get into it:
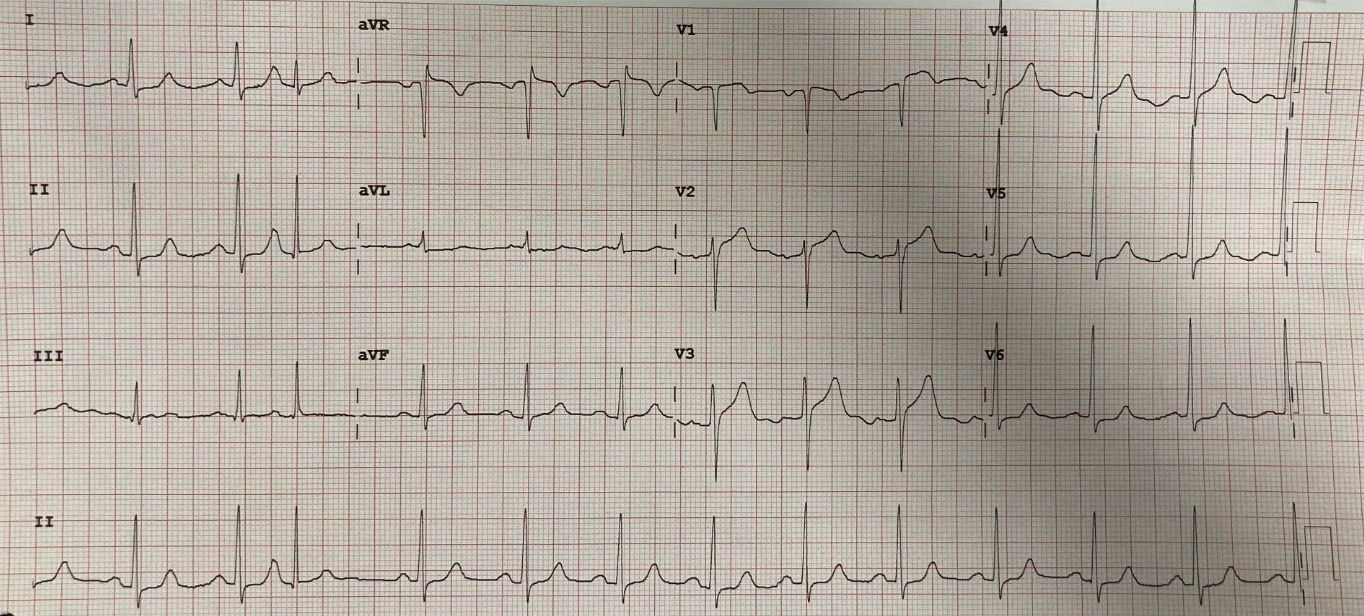
You’re working in the trauma bay and a tech hands you this ECG:
This veteran tech informs you the patient is a 71 M with a PMH HTN who is coming in for 1 week of intermittent chest pain and that he appears uncomfortable.
What is your next step?
A) Activate STEMI
B) See the patient immediately
C) Send the patient to the main ED with telemetry monitoring
D) Send the patient back to the waiting room
You see the patient immediately and he looks like this:
He appears uncomfortable, is diaphoretic, and clutching his chest. You obtain more history from his son: 71 M PMH HTN presents for 1 week of intermittent chest pain. Pain is nonexertional, nonpleuritic, and nonradiating. Over the past 30 minutes, the pain has acutely worsened, has become constant, and is now associated with diaphoresis and 1 episode of vomiting. This prompted the patient’s son to bring him to the ED.
Given this additional information, what do you want to do next?
A) Activate STEMI
B) Bring the patient to trauma bay to expedite care: draw labs, pain control, repeat ECG, bedside echo, and call cardiology emergently
C) Order labs and chest xray for the patient and send him to the main with telemetry monitoring
D) Send the patient back to the waiting room
Before divulging what happened next, let’s take a closer look at this ECG:
This is an interesting ECG to dissect because there are some subtle, yet concerning features:
ST elevations: Specifically in V2-V3 (the anterior leads). These STEs are around 2-3 mm in these leads, which fits STEMI criteria given his age. There are also subtle <1 mm STEs in V1 and aVR, which don’t quite fit STEMI criteria but are still concerning. Remembering our PAILS mnemonic, if we have STEs in the anterior leads, we should expect to see reciprocal depressions in the INFERIOR leads
ST depressions: There does appear to be a SLIGHT <1 mm ST depression in lead II, but none in lead II or aVF. Interestingly, we do see ST depressions in other leads….
The lateral leads: Interestingly, we do see some subtle <1 mm depressions in the LATERAL LEADS (specifically I, aVL, and V6). The does not exactly fit with the anterior STEs, as we would expect to see lateral depressions in an INFERIOR STEMI. This is something to keep an eye on as well.
STEMI Criteria (left). Source: https://www.tamingthesru.com/blog/grand-rounds/stemi
PAILS Mnemonic (right) - Where to expect reciprocal depressions in STEMI. Source: https://lightssirensactionems.com/blogs/news/tagged/ecg
To me, this ECG does not quite meet STEMI criteria, however….
Taking the whole picture into consideration, STEMI is activated. REMEMBER: YOU ARE NEVER WRONG TO ACTIVATE STEMI IF YOU ARE CONCERNED!
The patient is brought to the trauma bay. Labs are drawn and a repeat ECG is obtained 10 minutes later. The initial ECG is provided for comparison.
Patient’s initial ECG (left) and repeat 10 minutes later (right)
OOF! Good thing we repeated the ECG because it looks BAD.
ECG#1 was scary, but there are some DYNAMIC CHANGES on ECG#2 that make it even scarier!
Worsening STEs in anterior leads: Initially the patient had around 2 mm STEs in V2 and V3 and <1 mm STEs in aVR and V1. BUT repeat showed more pronounced STEs in these leads and NEW STE in V4. The morphology of the STEs in ECG #2 are also much scarier
Worsening ST depressions: With elevations in the anterior leads, we would expect to see reciprocal depressions in the inferior leads. The initial ECG showed a SLIGHT depression in lead II, but the repeat had much more convincing reciprocal depressions in II with a new ST depression in aVF
Dynamic changes in lateral leads: Interestingly, the initial ECG showed slight depressions in I, aVL, and V6 (which we would expect to see in an inferior STEMI). On repeat, the ST segments in I and V6 appear flatter. This does not classically fit with the anterior STEMI pattern, but patients don’t read the textbooks and any dynamic changes should raise alarm bells.
Back to the Patient:
Bedside echo was performed and showed anterior regional wall abnormalities. The patient was taken immediately to cath lab and found to have a 100% mid-LAD occlusion and severe proximal LAD stenosis. 2 LAD stents were placed. The patient is now fully recovered.
Take Home Points:
Trust your techs: Remember they are seeing the patient first. In this case, the tech voiced his concerns and the team appropriately saw the patient immediately
See the patient immediately if the ECG looks funny: You can get a better history to help guide management. Even just eyeballing the patient can give you important context clues…
Diaphoresis = BADNESS: Patients can’t fake diaphoresis- if you see a sweaty patient, you should be concerned
Obtain a repeat ECG: If the first ECG and/or the story are alarming, obtain a repeat to look for dynamic changes
When in doubt, ACTIVATE STEMI: You are never wrong to activate STEMI if you’re concerned. Get cardiology on board at let them decide if and when they want to cath the patient