Posterior Tibial Nerve and Sural Nerve Block
Written by: Kyle Soldevilla, DO Edited by: Nathan Zarider, MD
Case
A 65 year old male presents to your emergency department after being sent in from his podiatrist. He states that he was exercising this morning and attempting to move some equipment around on the floor when his left foot got caught on a screw sticking out from a pull up bar. He went to his podiatrist who attempted to repair his laceration, but he was unable to tolerate the procedure in the office. His podiatrist has already injected the surrounding area liberally with lidocaine and partially repaired the wound, however a large portion still remained untouched. The laceration is approximately 4 cm long, 3 mm deep, and is isolated to the plantar aspect of his foot. The laceration extends laterally to medially as illustrated below:
Given patient received local anesthetic (LA) just prior to arrival, a nerve block is considered as it will give a large field of anesthesia and limit total dose of LA to avoid toxicity.
Anatomy
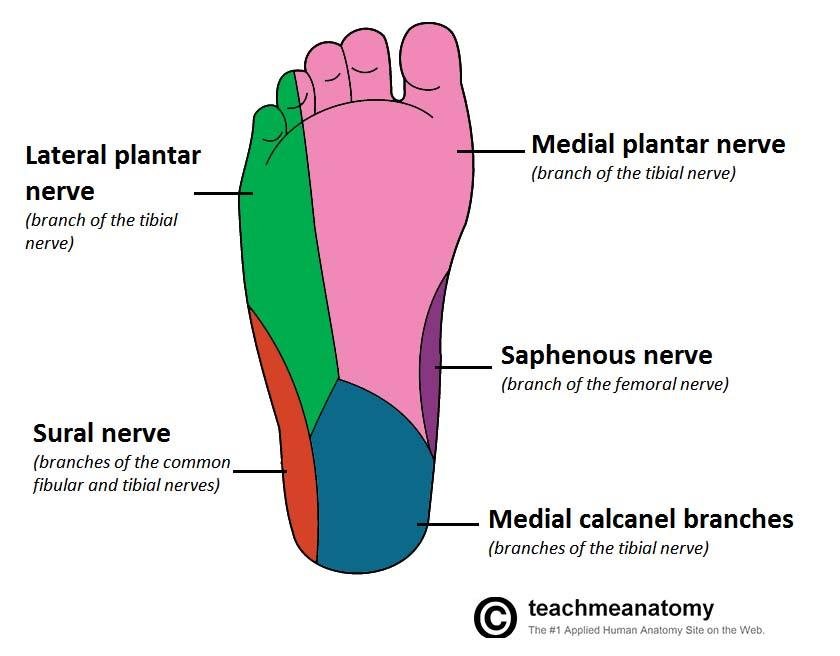
In order to adequately anesthetize the area of injury, our nerves of interest are the posterior tibial nerve (branch of sciatic nerve) and the sural nerve (branch of femoral nerve). As seen in the diagram, the vast majority of sensory innervation to the plantar surface of the foot is delivered by the lateral plantar nerve, medial plantar nerve, and medial calcaneal branches (which are all smaller branches of the posterior tibial nerve that split after the tarsal tunnel). Thus, we can anesthetize most of the injured area with just a single block.
The final area of interest is the sural nerve. The sural nerve is a small sensory nerve with no motor function that supplies the lateral aspect of the foot and lower leg as seen in the figures, anesthetizing the rest of our area of interest.
Visualizing and blocking the posterior tibial nerve
Key landmarks: the medial malleolus and posterior tibial artery
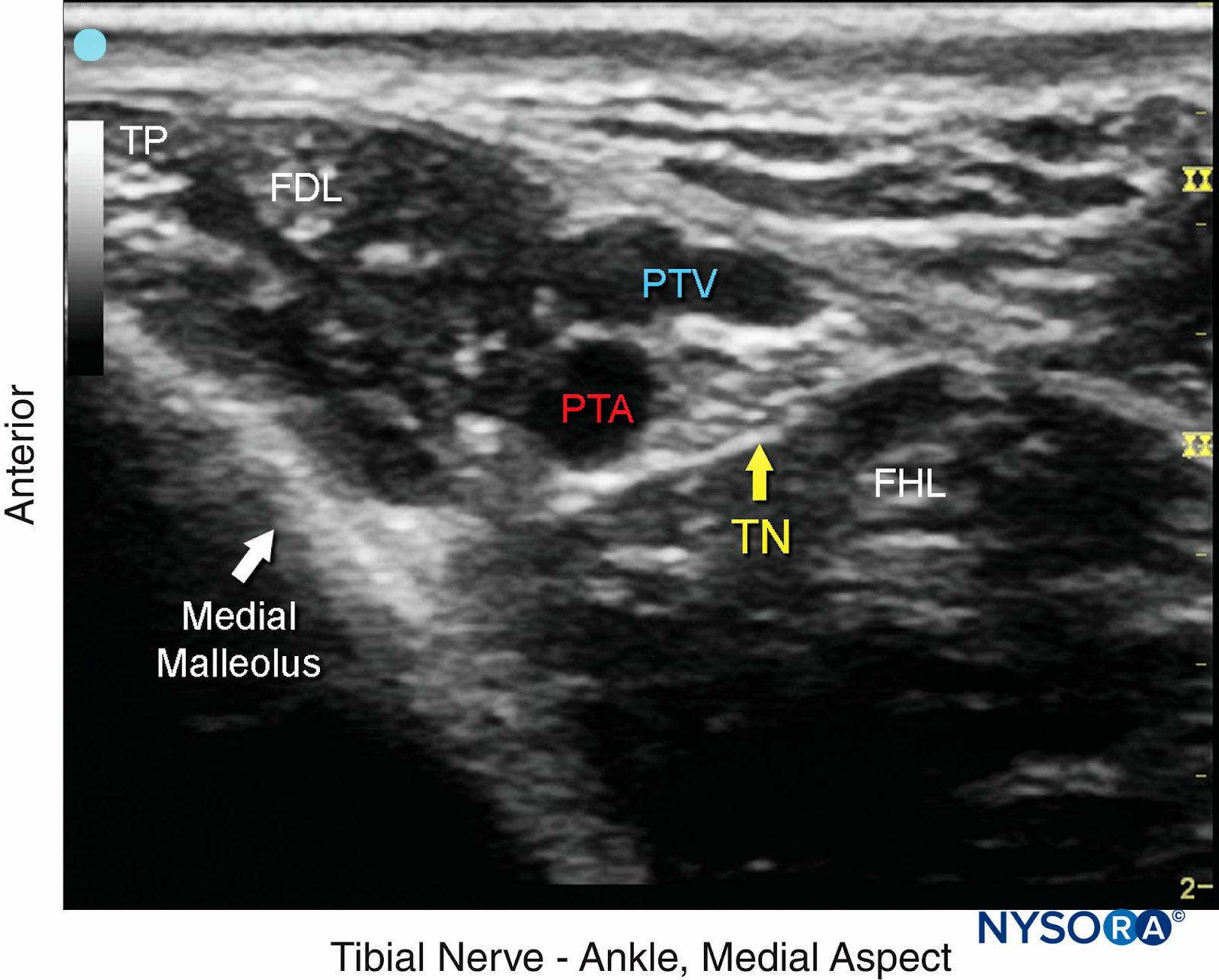
Using the linear probe, orient your probe in the transverse plane just superior to the medial malleolus with the probe marker towards patient anterior. Your anatomical area of interest is the area just superior to the tarsal tunnel which should appear as figure A.
Figure A: Tibial Nerve block superior to tarsal tunnel
There will be other various tendinous structures that you may confuse with the nerve, however the nerve should rest comfortably posterior to the to the posterior tibial artery and vein. All structures include (in the anterior to posterior direction): tibialis posterior, flexor digitorum longus, posterior tibial artery/vein, posterior tibial nerve, and flexor hallucis longus.
Needle approaching L posterior tibial nerve
Posterior tibial nerve bathed in LA w/ adjacent fascial spread
Visualizing and blocking the sural nerve
Key structures: Achilles tendon, sural nerve, small saphenous vein, peroneus brevis (most anterior)
Just opposite of the posterior tibial nerve block is the sural nerve block. Again with the probe in transverse, place the US probe in lateral position oriented slightly posterior and superior to the lateral malleolus. The probe marker should be facing anteriorly. Structures that should be in view include (from anterior to posterior): peroneus brevis muscle, sural nerve, small saphenous vein, and Achilles tendon.
Ultrasound probe positioning for Sural nerve block
Sural nerve pathway
Sural nerve bathed in LA w/ adjacent fascial spread
Due to the small size of this nerve, it is frequently difficult to visualize. You can attempt to increase the size of the vein by applying a calf tourniquet to optimize visualization as the nerve is typically in its immediate vicinity. Alternatively, if it remains difficult to visualize, you may opt to inject lidocaine as a “subcutaneous skin wheal” from the lateral achilles tendon to the medial malleolus to block this distribution. This method is equally as effective given the superficial position of this nerve.
As with all procedures, informed consent should be obtained and sterile precautions taken. Using an in-plane technique, insert a 20 g needle in the posterior-to-anterior direction and guide the needle to the nerve. Inject 1-2 ccs of sterile saline to confirm proper injection plane through visualization of fascial spread and vascular spreading from the nerve. Once location is confirmed, 2-5 ccs lidocaine 2% will suffice to anesthetize each region.
Back to the case…
After prompt performing of both nerve blocks, the patient was re-evaluated and reported zero sensation of pain on sensory testing. The patient was able to tolerate full wound irrigation and a 16 stitch laceration repair with no difficulty or complications.
References:
http://highlandultrasound.com/tibial-block