Erector Spinae Nerve Block for Renal Colic
By Mark Spoerer DO, Edited by Jeff Greco MD
Case
A 27 year old female presents herself to your emergency department with sudden onset severe left flank pain that has persisted for 3 hours. Patient states that she has a history of kidney stones and nothing seems to ever relieve her pain. She already took 975mg of Tylenol before arrival. She additionally notes that she cannot take opioids anymore due to “too much fun she had in her early 20s”. Patient is also 10 weeks pregnant and is afraid anything we give her could harm her baby. You then decide to whip out your handy dandy ULTRASOUND! You immediately notice hydroureteronephrosis and suspect an obstructing kidney stone. After ruling out other pathology, your patient is crying out in pain and asking for help. You remember reading online about a novel idea for a nerve block to alleviate renal colic. After a discussion with the patient you both decide the nerve block is your best option.
Erector Spinae Plane (ESP) Nerve Block
Is a nerve block where anesthetic such as bupivacaine or lidocaine, is injected below the Erector Spinae. This technique is relatively new and is theorized to act by either an anterior diffusion of the local anesthetic into the paravertebral space or possibly through an interfascial spread toward the posterior rami of the spinal nerves.
Location, Location, Location
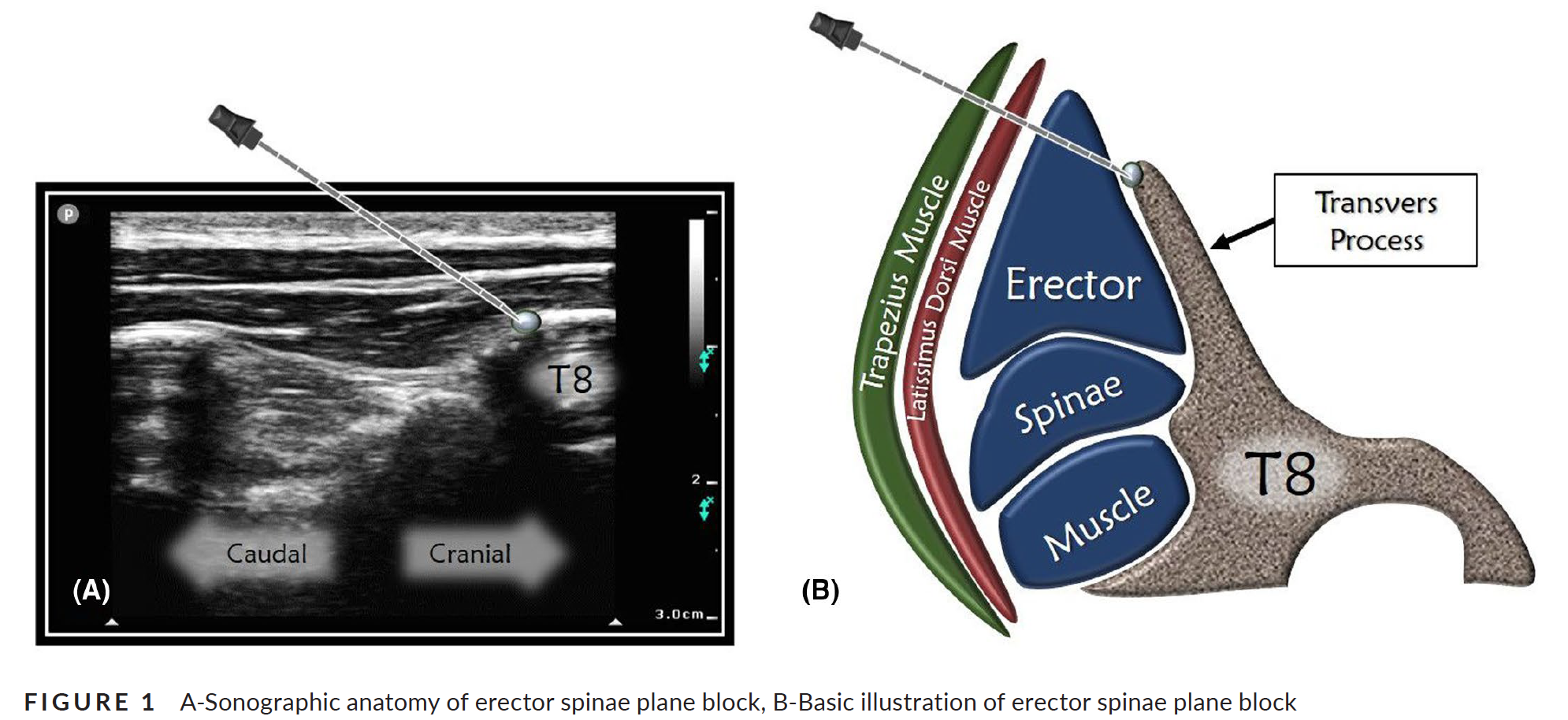
Just as with any nerve block, the location of your injection is paramount! Your injection is best placed just below the erector spinae muscles over the transverse process of the spine in the level of desired effect as shown to the right.
For renal colic there have been case reports showing relief of pain with an ESP block in the T8 transverse process on the side of the pain. There does not seem to be evidence on whether a cranial or caudal approach is best and the image below shows a caudal approach in contrast to the one to the right.
The Actual Procedure
As with all procedures, consent should be obtained, and sterile precautions should be taken. Insert the needle in-plane from a cranial to caudad direction until the needle tip contacts the transverse process. Inject 1-3 mL of local anesthetic to confirm proper injection plane by visualization of a spread deep to the erector spinae muscles and superficial to the transverse process. Complete the nerve block with 20-30 mL of local anesthetic.
Back to the case…
After performing your ESP block the patient's pain is completely relieved! “Doc I will be coming to you every time I have a kidney stone!” The patient was found to have a 1 cm stone in the left mid ureter in the MRI and taken for stent placement and lithotripsy.
Case Reflection
Renal colic has been a major contributor to the opioid epidemic and the ESP block can provide a fast acting and non addictive alternative to opioids. In one prospective randomized study that included only 40 patients, Those that received an ESP block drastically preferred it over NSAIDs for pain relief. Due to the new introduction of this technique and its scarcity of use, consequences and complications have not been well established. With the limited evidence so far this technique should be kept in the back of your mind for those patients that don’t seem to improve with the standard of care as a possible safe alternative.
References
Erector Spinae Plane Nerve Block - NYSORA. NYSORA. Published February 11, 2021. Accessed April 9, 2021. https://www.nysora.com/erector-spinae-plane-block/
Aydin ME, Tekin E, Ahiskalioglu EO, et al. Erector spinae plane block vs non‐steroidal anti‐inflammatory drugs for severe renal colic pain: A pilot clinical feasibility study. International Journal of Clinical Practice. 2020;75(3). doi:10.1111/ijcp.13789
Tozer J. JournalFeed. JournalFeed. Published March 26, 2021. Accessed April 9, 2021. https://journalfeed.org/article-a-day/2021/new-nerve-block-for-renal-colic
Nikiforov S, Cronin Arthur J, Murray W Bosseau, Hall Virginia E. Subcutaneous Paravertebral Block for Renal Colic. Anesthesiology. 2001;94(3):531-531. doi:10.1097/00000542-200103000-00027