Stellate Ganglion Nerve Block
Written by: Omar Hilal, MD. Edited by: Jeff Greco, MD
The CASE
A recent case report from Annals of Emergency Medicine [1]:
65 yo male with PMH of HTN presents with acute chest pain and SOB
Rhythm strip in field concerning for STEMI with elevations in leads I, V2-V4
Patient become unresponsive and pulseless in hospital with V-tach on monitor
Patient underwent CPR for approximately 40 min with continuous chest compressions, defibrillated with 200J during shockable rhythms, given multiple rounds of epinephrine, sequential doses of amiodarone, magnesium, bicarb were given. Esmolol was also started to no avail.
After considering calling the resuscitative efforts, stellate ganglion block done on the left sympathetic chain with US guidance after which 1 more round of compressions and defibrillation was done with ROSC achieved. ECG showed accelerated idioventricular rhythm.
In this case, belief is that the blunted sympathetic response made the patient more responsive to the CPR interventions meant to halt ventricular arrhythmia
Patient ended up with 2 stents to LAD as he had total occlusion.
Despite protracted 45 day hospital course, peak troponin level of 162.1 ng/ml, markedly reduced left ventricular EF of 35%, and temporary dependence on percutaneous ventricular assist device, patient able to be DC’d to subacute rehab and experienced full neurologic recovery.
What, pray tell, is the Stellate Ganglion?
An oval shaped structure that is the product of the fusion of inferior cervical and first thoracic sympathetic ganglions
Located anterior to the neck of the first rib and anterolateral to the longus colli muscle
Anterior to the transverse process and prevertebral fascia.
Vertebral vessels, carotid artery, superior intercostal artery, trunk of the subclavian artery all surrounding structures.
Its somatic branches provide sympathetic fibers to the anterior rami of C7, C8, T1 with the visceral branches contribute to the cardiac plexus.
[2]
Clinical significance
Typically a target of nerve blockade for diagnostic and therapeutic purposes [3]
[4]
Refractory cardiac arrhythmias
CRPS - Complex regional pain syndrome
Refractory angina
Atypical angina
Phantom limb pain
PTSD - Post-traumatic stress disorder
Neuropathic pain syndromes
Cluster and migraine headaches
Raynauds
Scleroderma
Meniere's syndrome
Quinine poisoning
Diagnosis of sympathetic mediated pain
[5]
How do you know you’ve successfully completed the nerve block?
[6]
Look for signs of sympathetic chain blockade:
Miosis
Anhidrosis
Ptosis
Flushing of extremities
Rise in upper extremity temp 1-3 degrees
Symptoms usually disappear 4-6 hours after blockade
What are some risks?
Pneumothorax
Phrenic nerve blockade with diaphragmatic paralysis
Recurrent laryngeal nerve blockade
HTN
Hematoma
Seizures
Paratracheal hematoma
The Procedure
How would one do this block if they were so inclined, you say?
US guided C6 transverse
Carotid sheath and SCM muscles retracted laterally with probe
Gentle pressure to reduce distance between skin and tubercle
Needle inserted towards Chassaignac tubercle
After needle contacts tubercle, retracted 1-2mm in the area of prevertebral fascia
2ccs of anesthetic injected with visualization to confirm that you are sub-fascial
Remainder of anesthetic administered
US guided C7 anterior approach
Higher risk of PTX or vertebral artery injury but more consistent blockade
Probe placed transverse over trachea and moved laterally at level of C6
Carotid artery, thyroid gland, and longus colli muscle visualized
Inject at point posterior to carotid artery over the pre-vertebral fascial plane
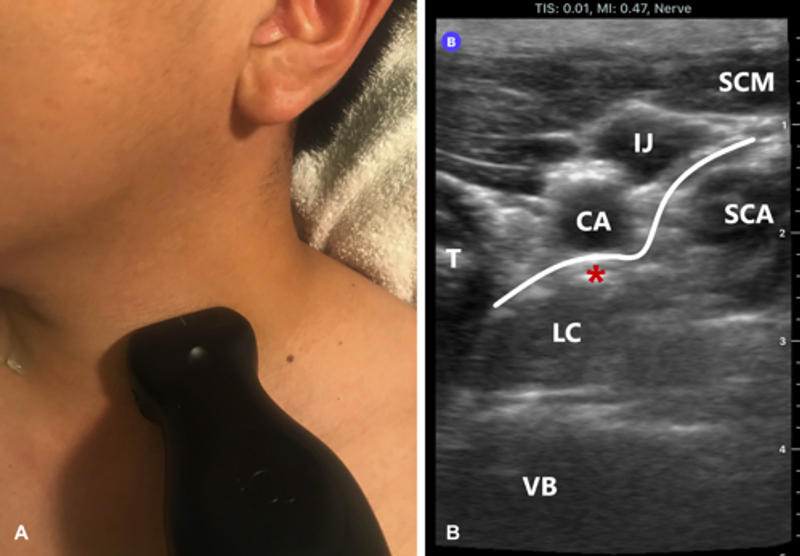
A. High-frequency linear array transducer should be placed in the left anterior paratracheal region just below the area of the thyroid notch.
B. Injection of 10 mL of lidocaine should occur underneath the pretracheal fascia above the longus colli muscle (asterisk).
CA, Carotid artery; IJ, internal jugular vein; LC, longus colli muscle; SCA, anterior scalene muscle; SCM, sternocleidomastoid muscle; T, thyroid; VB, vertebral body; white line, pretracheal fascia [7]
Does it really work?
WHO KNOWS? KEEP IT IN MIND THO IF NOTHING ELSE DOES
References:
[1] https://www.annemergmed.com/article/S0196-0644(19)30612-2/fulltext?dgcid=raven_jbs_etoc_email
[2] Stellate Ganglion Block | Vascular & Visceral Pain Treatment
[3] Neuroanatomy, Stellate Ganglion - StatPearls
[5] https://www.youtube.com/watch?v=t_0187wBdLA
[6] https://www.youtube.com/watch?v=t_0187wBdLA
[7] https://www.annemergmed.com/article/S0196-0644(19)30612-2/fulltext?dgcid=raven_jbs_etoc_email

![[2]](https://images.squarespace-cdn.com/content/v1/5bc94f5b9b7d1515843688af/1582136287004-IASLEUCV5BAMGOGJVHKM/Picture1.png)
![[4]](https://images.squarespace-cdn.com/content/v1/5bc94f5b9b7d1515843688af/1582136385337-8FHOZKWIKX2MQ238JJPJ/2.png)
![[5]](https://images.squarespace-cdn.com/content/v1/5bc94f5b9b7d1515843688af/1582136436225-MU8BVI0YWEFWH2SHE88D/3.png)
![[6]](https://images.squarespace-cdn.com/content/v1/5bc94f5b9b7d1515843688af/1582136450040-O2GAIRVSJFH99WK5B58S/4.png)