Oh MAN! - Interstitial Ectopic
Megan Varghese, MD PGY-1
Edited by: Nathan Zardier, MD
Case
Patient is a 42 year old woman, G6P5005 F at 7wks4d by LMP. One week prior she presented to the emergency department. At that time TVUS showed IUP w/ gestational sac and yolk sac. A FHR was noted and the crown-rump length was consistent with dates. HCG was 54,000 at that time. She was sent to the ED after in-office follow up with OB w/ repeat ultrasound in clinic were concerning enough to warrant possible surgery. HCG quant from clinic showed HCG was 85,000 today. She denies vaginal bleeding, abdominal pain, prior hx of PID/STI, prior hx of ectopic pregnancy. No prior gynecologic surgeries. She is asymptomatic.
Her exam is completely normal.
What concerned her OBGYN enough to send her in urgently for evaluation?! Her OB was concerned for possible interstitial ectopic pregnancy.
Ectopic Pregnancy - Background
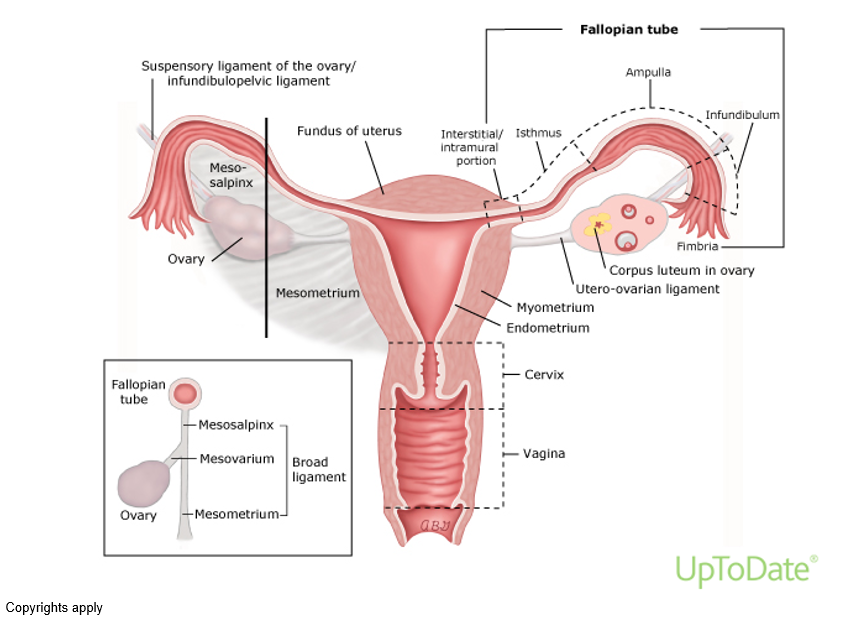
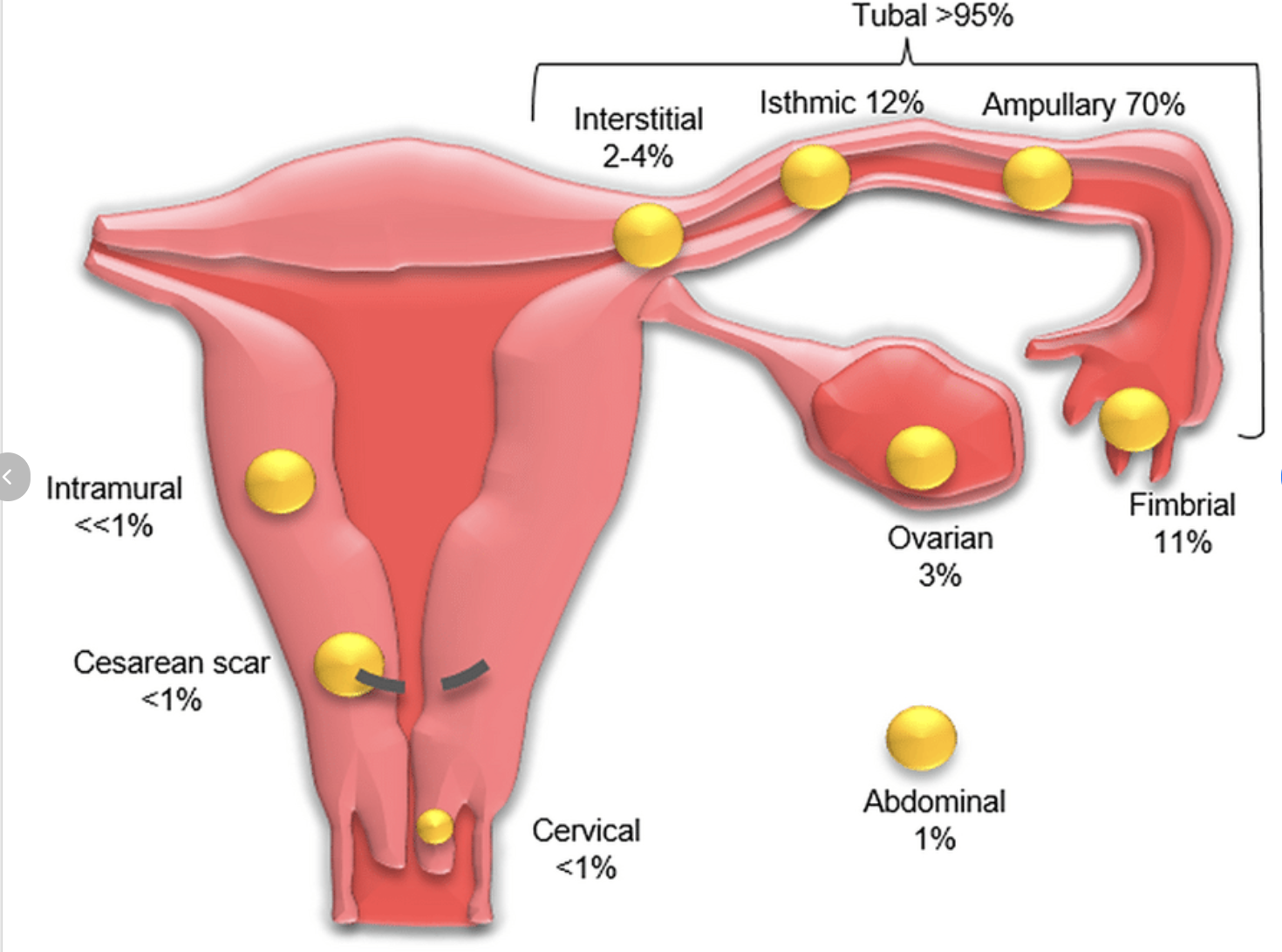
A ruptured ectopic pregnancy is a surgical emergency, and the leading cause of maternal mortality in the first trimester. Sources attempting to determine incidence of ectopic pregnancy vary, but they are thought to complicate less than 1% of all pregnancies(Uptodate). However, in women presenting to the ED with abdominal pain, vaginal bleeding, and amenorrhea - rates are much higher. One retrospective study of 2,026 patients presenting to the ED with vaginal bleeding in the first trimester showed that 18% of these presentations had ectopic diagnosed. The most common presenting complaints were vaginal bleeding and abdominal pain.2 The are most commonly found in the ampulla of the fallopian tube, then the isthmus and fimbria, and less commonly seen in the interstitium of the fallopian tube, ovary, abdomen, and in the abdomen/cervix.
Risk factors for an ectopic pregnancy include a prior ectopic, PID, IUD, prior tubal surgery, and advanced maternal age. Symptoms present 6-8 weeks after LMP and include but are not limited to abdominal pain (acute or chronic), vaginal bleeding, amenorrhea, and phys exam can reveal cervical motion tenderness, adnexal TTP, while a RUPTURED ectopic may present with signs of hemorrhagic shock, vaginal bleeding and abdominal pain.
Role of US in the ED:
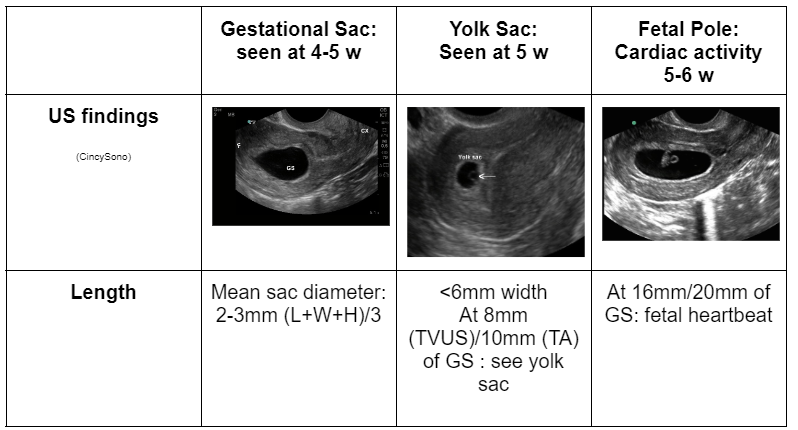
Diagnosis of ectopic pregnancy can be difficult as symptoms can range from asymptomatic, to mild abdominal pain and vaginal spotting, to florid hemorrhagic shock, hypotension and profuse vaginal bleeding. The best approach to evaluation of ectopic is to perform a transvaginal ultrasound to aid with diagnosis as it provides higher resolution images of the uterine cavity at lower HCG thresholds (Discriminatory threshold for HCG level is ~2,000 IU). Sensitivity and specificity of transvaginal ultrasound at diagnosing ectopic pregnancy in those with HCG of 2000 or greater is 10.9% and 95.6%, respectively.3 Therefore ultrasound cannot rule out ectopic. Instead, you’re goal is torule IN an IUP.
Ultrasound Findings in IUP:
Interstitial Ectopic Pregnancy
Interstitial ectopic pregnancies are also known as cornual ectopic pregnancies. They implant at the junction of the proximal most fallopian tube and also within the myometrium. They are often eccentrically located within the uterus and easily confused for an intrauterine pregnancy. If misdiagnosed, they can grow and rupture. The main risk factor is prior intrauterine instrumentation. ((4)“Interstitial and Cornual Ectopic Pregnancy: Conservative Surgical and Medical Management”)
Use of POCUS - Endomyometrial MANtle
A normal IUP (AliEM)
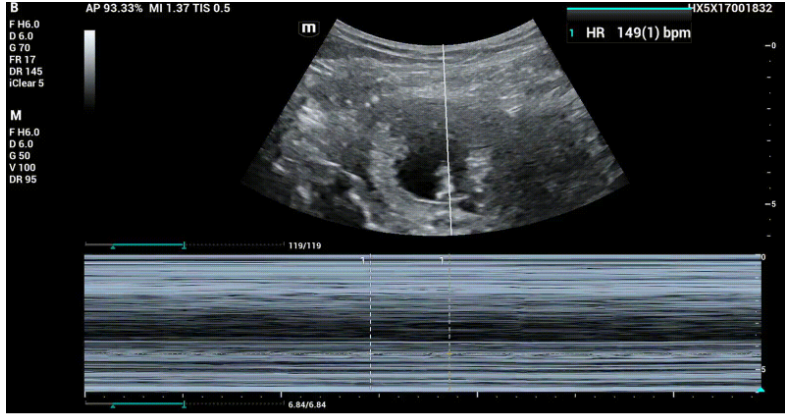
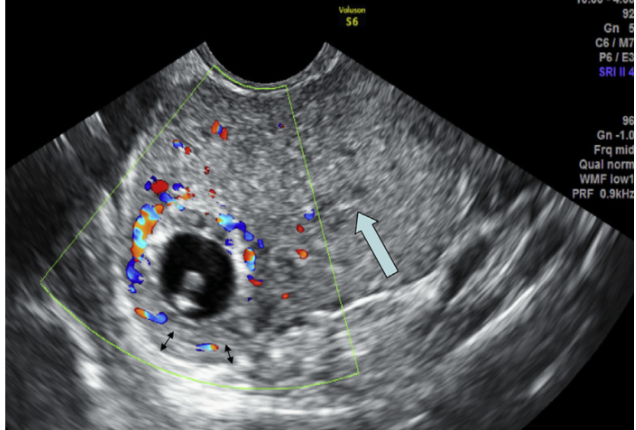
Our patient’s TAUS:
Here we see a GS, YS and FP, but observe how thin the distance between the GS and outer uterine wall is (at approximately 3 cm depth)
Fetal cardiac activity w/ FHR = 149 as seen with M-mode.
The main finding for an interstitial ectopic is an abnormally eccentric gestational sac and thin surrounding myometrium: "endomyometrial mantle". The endomyometrial mantle measurement that indicates abnormal implantation varies in different studies but generally, <5 mm is highly suspicious for interstitial pregnancy while <8 mm is more sensitive but less specific. (5. (Interstitial ectopic pregnancy,Lin TY))
Here we measure from the wall of the gestational sac to the outer wall of the uterus, and confirm if the mantle is <8 mm.
Interstitial Line Sign & Ring of fire
Interstitial line finding in interstitial ectopic pregnancy (6).
To increase the predictive value of US for making an Interstitial ectopic pregnancy diagnosis, research was done on use of the interstitial line sign: visualizing a thin, echogenic line that extends from the central uterine cavity echo to the periphery of the interstitial gestational sac. The line represents the endometrial canal or the interstitial portion of the fallopian tube. When used in combination with the mantle <8 mm and eccentric sac location, the interstitial line sign may provide a useful clue for the early diagnosis of interstitial pregnancy.
Ring of fire: peripheral vascularity seen in ectopic pregnancies, not specific. Can be seen commonly in corpus luteum cysts, so care must be taken when interpreting this finding especially if ovarian ectopic is suspected.
Management
Interstitial Pregnancies are treated either with medical/surgical management in consultation with OB/GYN. Medical management involves administration of methotrexate 50 mg/m^2 either systemically/injected into the gestational sac, or a combination of the two. Surgical management can requires with cornual wedge resection and salpingectomy. (7) Our patient from this case had a R abdominal salpingectomy and R cornual wedge resection, and post-op course was uncomplicated.
References
3. Diagnostic accuracy of varying discriminatory zones for the prediction of ectopic pregnancy in women with a pregnancy of unknown location - PubMed. Accessed December 4, 2022. https://pubmed.ncbi.nlm.nih.gov/16308901/
4. Dagar M, Srivastava M, Ganguli I, Bhardwaj P, Sharma N, Chawla D. Interstitial and Cornual Ectopic Pregnancy: Conservative Surgical and Medical Management. J Obstet Gynaecol India. 2018 Dec;68(6):471-476. doi: 10.1007/s13224-017-1078-0. Epub 2017 Nov 28. PMID: 30416274; PMCID: PMC6207538.
5. Lin TY, Chueh HY, Chang SD, Yang CY. Interstitial ectopic pregnancy: A more confident diagnosis with three-dimensional sonography. Taiwan J Obstet Gynecol. 2021 Jan;60(1):173-176. doi: 10.1016/j.tjog.2020.11.028. PMID: 33494997.
6. Ackerman TE, Levi CS, Dashefsky SM, Holt SC, Lindsay DJ. Interstitial line: sonographic finding in interstitial (cornual) ectopic pregnancy. Radiology. 1993 Oct;189(1):83-7. doi: 10.1148/radiology.189.1.8372223. PMID: 8372223.
7. Kahramanoglu I, Mammadov Z, Turan H, Urer A, Tuten A. Management options for interstitial ectopic pregnancies: A case series. Pak J Med Sci. 2017 Mar-Apr;33(2):476-482. doi: 10.12669/pjms.332.12093. PMID: 28523060; PMCID: PMC5432727.