An abnormal infant gallbladder
Written by: Eugene Borst, MD
Edited by: Joann Hsu, MD
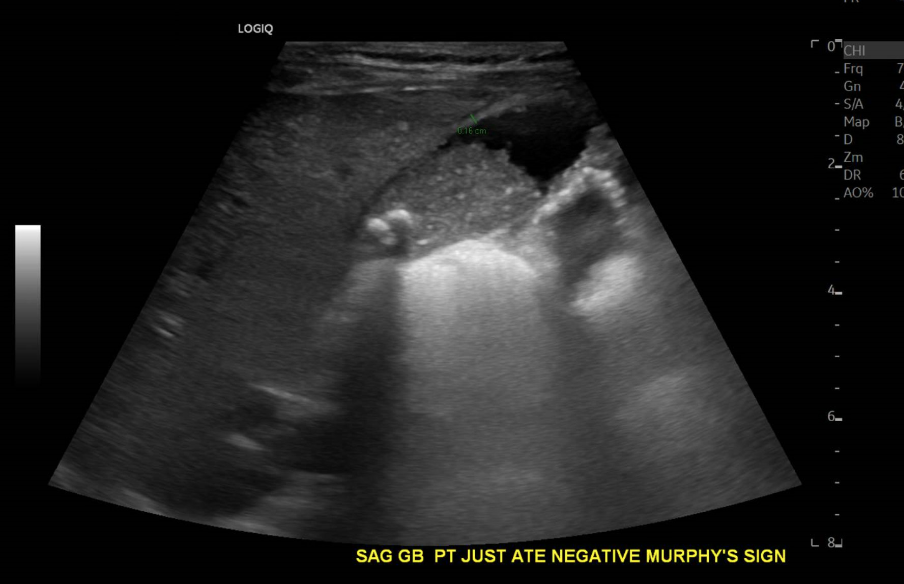
A 16 month-old female with no prior medical history was sent to the ED by her primary care provider for elevated liver enzymes. Her mother states that everyone in the household had symptoms of a viral illness two a week and a half before. The patient had a fever of 102 two days ago but no fevers since. Her mother also noticed gray stool in the patient’s diaper starting around the same time. The patient is otherwise asymptomatic with no changes in feeding or behavior.
Bedside right upper quadrant ultrasound revealed…
A comprehensive ultrasound was performed. The report read:
“Large amount of gallbladder sludge and multiple shadowing stones in the gallbladder neck. The gallbladder is distended and there is dilation of the cystic duct and common bile duct, consistent with biliary obstruction.”
“Apparent septated area at the gallbladder neck communicating with the gallbladder, likely reflecting a dilated tortuous cystic duct or honeycomb gallbladder morphology. Sludge is seen within this structure.”
“Mildly increased parenchymal echogenicity of the liver, nonspecific.”
So why does a baby have this gallbladder?
Progressive Familial Intrahepatic Cholestasis
Part of a heterogeneous group of disorders.
Characterized by defective bile acid or bile acid secretion.
Usually present in infancy or early childhood but can present any time in a patient’s life.
Associated w/ growth failure liver disease and many have coagulopathies (vitamin k malabsorption).
Are considered “orphan diseases”
PFIC TYPE 3
Error in gene that is proposed to replace phosphatidylcholine in the outer lipid membrane of the bile canaliculus.
Bile salt secretion remains normal.
Leads to damage of the canalicular membrane -> progressive destruction of smile bile ducts.
Elevated ggt is the distinguishing characteristic.
References
1. 5 Minute Sono - Core Ultrasound. Published February 14, 2019. Accessed November 6, 2023. https://coreultrasound.com/5ms/
2. Singh G. Biliary atresia | Radiology Reference Article | Radiopaedia.org. Radiopaedia. doi:10.53347/rID-5176
3. Murray M. Honeycomb gallbladder | Radiology Case | Radiopaedia.org. Radiopaedia. doi:10.53347/rID-160125
4. Sundaram V, Björnsson ES. Drug‐induced cholestasis. Hepatol Commun. 2017;1(8):726-735. doi:10.1002/hep4.1088
5. Gottesman LE, Del Vecchio MT, Aronoff SC. Etiologies of conjugated hyperbilirubinemia in infancy: a systematic review of 1692 subjects. BMC Pediatr. 2015;15:192. doi:10.1186/s12887-015-0506-5
6. JANSEN P, MULLER M. Progressive familial intrahepatic cholestasis types 1, 2, and 3. Gut. 1998;42(6):766-767.
7. de Vree JML, Jacquemin E, Sturm E, et al. Mutations in the MDR3 gene cause progressive familial intrahepatic cholestasis. Proc Natl Acad Sci U S A. 1998;95(1):282-287.
8. Jacquemin E, Hermans D, Myara A, et al. Ursodeoxycholic acid therapy in pediatric patients with progressive familial intrahepatic cholestasis. Hepatol Baltim Md. 1997;25(3):519-523. doi:10.1002/hep.510250303
9. Englert C, Grabhorn E, Richter A, Rogiers X, Burdelski M, Ganschow R. Liver transplantation in children with progressive familial intrahepatic cholestasis. Transplantation. 2007;84(10):1361-1363. doi:10.1097/01.tp.0000282869.94152.4f