Bronchiolitis Ultrasound Score
Written by Alex Chu, MD. Edited by Jeff Greco, MD.
You are alone at night in the middle of the winter influenza/covid season and you receive a notification from EMS that they are bringing you a febrile, coughing 6 month old male.
Upon arrival, you find a tearful mother holding her crying child. She states that he is fully vaccinated and previously healthy but developed a fever of 102 F axillary with cough and runny nose that started 5 days ago. She gave him tylenol 8 hours ago, but it didn’t break his fever and she’s worried he’s getting worse. He isn’t eating as well and isn’t making as many wet diapers as usual. He has an older sister in daycare at home, but she has been fine.
Vital signs are temperature 101 F rectal, heart rate 190 bpm, respiratory rate 32, blood pressure 90/60, oxygen saturation 97%, weight 8 kg.
His physical examination is remarkable for intermittent cough with mild wheezing and rhinorrhea.
Chest x-ray is performed and there is no focal consolidation noted. Urinalysis is performed and negative for UTI. Respiratory pathogen panel is performed and he is positive for respiratory syncytial virus (RSV).
He is given some fluids and seems to perk up a bit, but then vomits.
Okay…
Now, you’re left with a 6 month old previously healthy infant with bronchiolitis with an unclear disposition. Some people might admit him, while others might attempt other measures to see if he can be safely discharged home with close follow up.
But here’s where ultrasound can help.
Lung ultrasound has been popularized in the diagnosis of pulmonary conditions, particularly in the last decade. Multiple articles have discussed the utility of ultrasound in the diagnosis of bronchiolitis in pediatrics.
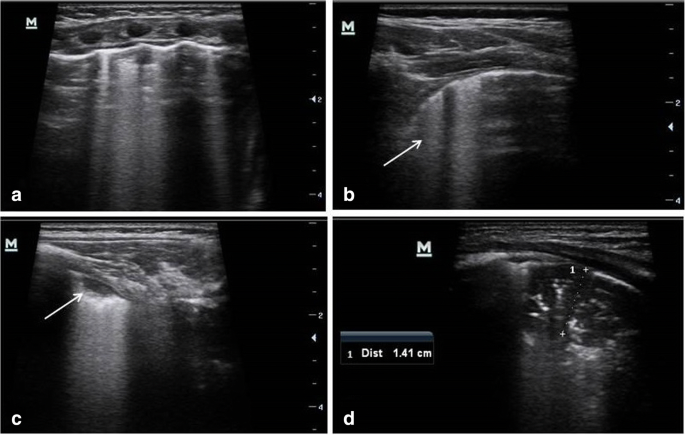
Supino et al performed a prospective study in the ED from 01/2017 to 03/2018 to determine whether lung ultrasound had any ability to predict need for interventions. Their study enrolled 76 infants suspected of having bronchiolitis. Subjects were first examined and then lung ultrasound was performed. They followed an ultrasound scoring system first proposed by Taveira et al. Each lung was divided into 6 quadrants (4 anterior, 2 posterior) and each quadrant was given a score of 0 to 2, with 0 being the healthiest, 1 being severe interstitial syndrome, and 2 being subpleural consolidation > 1 cm. Total maximum score is 24. Subjects were then given a clinical severity score based on the respiratory score criteria outlined in the bronchiolitis treatment pathway published by Seattle Children’s Hospital. They found there was a significant difference on ultrasound score between those that needed respiratory support and those that did not (p 0.003). They also discovered that their ultrasound score correlated with the duration of oxygen therapy during hospitalization (p 0.003, r 0.35) and the ultrasound score was higher in infants that needed respiratory support with HCPAP (p 0.028). Limitations included the fact that ultrasound has significant operator dependence and the number of infants with severe bronchiolitis involved in this study.
Image 1. Examples of ultrasound findings of bronchiolitis including B-lines, subpleural consolidation
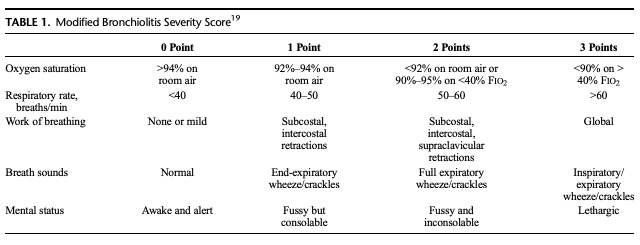
Ozkaya et al performed a prospective observation study that looked at the role of lung ultrasound in predicting the need for hospitalization in bronchiolitis patients. They looked at 76 infants with diagnosed bronchiolitis by two independent pediatricians and performed ultrasound to obtain a modified Bronchiolitis Severity Score and BUS score, outlined below.
They found that there was a significant correlation between the two scoring systems (r 0.698, p <0.001) and the BUS was the most effective parameter in determining admission on a logistic regression analysis (p 0.044, adjusted OR 1.859, 95% CI 1.016-3.404). Subjects with a BUS score of 3 or more had 73.81% sensitivity and 73.53% specificity for admission. Subjects with 4 or more had a 50% sensitivity and 91.18% specificity for admission. [2]
Given the above studies, it seems that properly performed LUS on bronchiolitis patients likely can shed some light onto the severity of disease reflected in the need for admission, need for respiratory support, and duration of respiratory support during hospitalization. However, further research should be performed to validate these findings in larger sample sizes and populations that are reflective of our practice environments.
Happy lunar new year!
Citations
Supino, Maria Chiara, et al. "Point-of-care lung ultrasound in infants with bronchiolitis in the pediatric emergency department: a prospective study." European journal of pediatrics 178.5 (2019): 623-632.
Özkaya, Ahmet Kagan, et al. "Lung ultrasound findings and bronchiolitis ultrasound score for predicting hospital admission in children with acute bronchiolitis." Pediatric emergency care 36.3 (2020): e135-e142.