Procedural Sedation
Written by: Vidhi Rao, MD; Edited by: Kent Li, MD
Background:
Procedural sedation is used for analgesia, anxiolysis, and/or brief immobilization during short procedures in the emergency department, often as an alternative to full operative anesthesia or in cases where operative management is not indicated. Procedural sedation increases patient comfort while also often decreasing costs and resources. Among both pediatric and adult patients with orthopedic complaints, there is data showing decreased time to reduction and decreased length of stay without associated increase in complication rates when using procedural sedation as opposed to general anesthesia in the operating room.
Target Level of Sedation:
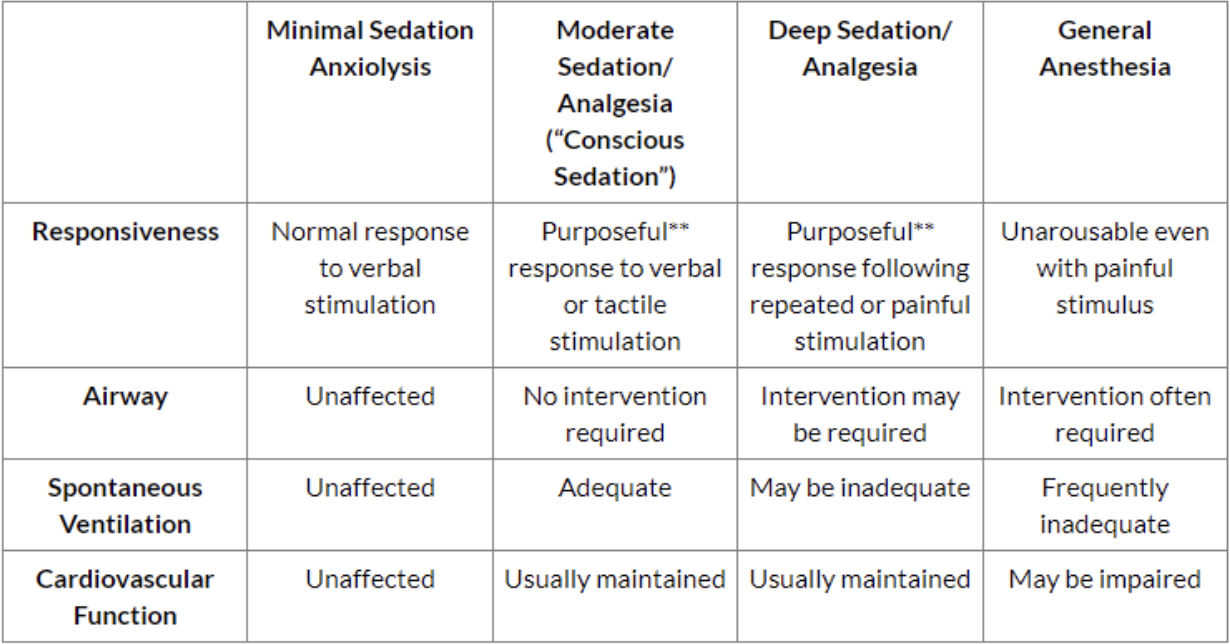
Before proceeding with procedural sedation, it is important to understand the different levels of consciousness and identify your target level of consciousness.
Fig 1: Target Level of Sedation. Note: Reflex withdrawal from painful stimuli is NOT considered a purposeful response. American Society of Anesthesiologists (ASA)
In the emergency department, procedural sedation can be used for numerous procedures, including but not limited to the following: reduction of dislocations or fractures, lumbar puncture, cardioversion, central line, tube thoracostomy, laceration repair, or imaging.
The target level of sedation depends both on the procedure and the patient’s needs; minimal or moderate sedation may suffice with simple procedures on a patient who is anxious but otherwise cooperative. Deep sedation may be more suitable for a patient who is unable to remain still (due to young age, mental status, distress, etc) or procedures that may induce significant discomfort/pain and result in involuntary movement/resistance, such as orthopedic reductions, which require muscle relaxation.
Hope for the Best, Prepare for the Worst:
Severe adverse outcomes rarely occur, and when they do they are most often within 30 minutes of the last administered dose. A systematic review showed the incidence of adverse events as follows:
Hypoxia: 40.2/1000
Vomiting: 16.4/1000
Hypotension: 15.2/1000
Aspiration: 1.2/1000
Laryngospasm: 4.2/1000
Intubation: 1.6/1000
Additionally, it has been shown that fasting does not decrease risk of emesis or aspiration in either the adult or pediatric population and thus procedural sedation, if appropriate, should not be delayed.
Predicting complications during sedation
Part of a complete H&P prior to procedural sedation includes assessing for past medical history of cardiovascular or respiratory problems and asking about allergies, both to medications and to foods (eg. propofol suspension contains soy, egg, and glycerol). The ASA classification categorizes patients based on their comorbidities; ASA III or higher are more likely to have complications and prolonged sedation time. Similarly, elderly patients are more sensitive to the medications used in procedural sedation and will have longer duration of hypoventilation and hypotension, hence the adage “start low and go slow”.
ASA classification
ASA I- A normal, healthy patient
ASA II- A patient with mild systemic disease
ASA III- A patient with severe systemic disease
ASA IV- A patient with severe systemic disease that is a constant threat to life
ASA V- A patient not suspected to survive without an operation
ASA VI- Brain dead patient
Preparing for airway catastrophe
While there’s no definitive way to identify which patients will have a challenging airway or require intervention at all, the following mnemonics may help you foresee potential problems:
BVM: ROMAN (Radiation/Restriction; Obstruction/Obesity/OSA; Mask seal/Male/Mallampati; Aged; No teeth)
Supraglottic device: RODS (Restriction; Obstruction/Obesity; Distorted anatomy; Short thyromental distance)
Direct Laryngoscopy: LEMON (Look externally; Evaluate 3-3-2; Mallampati; Obstruction/Obesity; Neck mobility)
Surgical airway (cricothyrotomy): SMART (Surgery; Mass; Access/Anatomy; Radiation; Tumor)
Additionally, any patient with a history of difficult intubation is more likely to be a difficult intubation in the future.
Finally, be ready to intervene! Preparation and set up should include:
Yankauer and suction set up
Non-rebreather mask and bag-valve mask (BVM) at bedside
Full range of airway tools unopened but ready
Nasopharyngeal/Oropharyngeal airway
Supraglottic airway and lubricant
Intubation materials (laryngoscope, endotracheal tube and stylet, syringe, back-up airway, etc)
If you do identify respiratory depression (example EtCO2 tracings shown later in this post), follow a stepwise approach
Stop medication and procedure
Head of bed 45’, sniffing position
Suction secretions
Jaw thrust
Apply pressure to laryngospasm notch if laryngospasm.
BVM + NPA, OPA
Supraglottic airway
RSI/intubation as last resort
It is important to note that in procedural sedation patients, hypoventilation is more likely than hypoxia and that BVM poses higher risk of emesis than in intubation because patient is not paralyzed. Early BVM is not the answer!
Image 1: Laryngospasm notch
And Now, the Drugs:
When choosing your medication(s), you should consider the duration of action, adverse effects, associated reversal agents, and whether the drug provides sedation or analgesia.
Sedatives (drowsiness)
Etomidate -- GABA receptor agonist that is uncommonly used due to short duration of action and associated myoclonus
Midazolam -- GABA receptor agonist that produces anterograde amnesia, anxiolysis, and spasmolysis. Note that adverse effects include respiratory depression as well as cardiovascular depression in hypovolemic patients or those with CHF
Propofol -- GABA receptor agonist that can cause respiratory depression and hypotension, especially with rapid administration. Have IV fluids ready for bolus.
Analgesia (pain relief)
Fentanyl -- potent CNS opioid agonist that produces analgesia and euphoria. The short-acting nature allows for ease of titration
Sedation + Analgesia (best of both worlds!)
Ketamine -- NMDA agonist that produces analgesia and amnesia without compromising respiratory drive, although there is risk of laryngospasm, hypersalivation, and apnea with rapid push. Other notable effects include emesis (particularly when administered IM), delirium and agitation due to emergence reaction, and theoretical increase in intracranial pressure. This latter concern has been debated in recent years; a 2020 systematic review found conflicting data regarding change in ICP and concluded that there is no evidence of ketamine-associated harm in acute brain injury patients.
Fig 2: Common Procedural Sedation Agents
Combinations
Fentanyl + midazolam
Higher doses of opioids can also produce a sedative-hypnotic effect, particularly when combined with another sedative-hypnotic, but this combination has been shown to have higher rate of pain and anxiety compared to other combinations and 4 times the risk of adverse respiratory events compared to midazolam alone
Fentanyl + propofol poses a similar concern about combining two respiratory depressants
Ketamine + midazolam -- complements!
Ketamine’s sympathomimetic activity reduces respiratory depression induced by midazolam. Meanwhile, midazolam theoretically decreases emergence reaction, a benefit shown in adults but not in children. The disadvantage of this combination is longer sedation time and slower recovery.
Ketofol -- synergy!
This combination produces a deeper level of sedation with less agitation and lower dosing of each. Additionally, propofol theoretically decreases emergence reaction, while ketamine’s sympathomimetic activity again counteracts cardiovascular and respiratory depression
Fig 3: Combination Sedation Regimens
Set Up: IV, O2, monitor, and EtCO2
All patients undergoing procedural sedation should have IV access and be hooked up to the monitor to look out for cardiovascular or respiratory compromise. In addition to cardiac monitoring with telemetry, timed blood pressure measurements, and pulse oximetry, end-tidal CO2 (EtCO2) should also be used. While there is conflicting evidence as to whether capnography reduces the rate of severe adverse airway events, it has been shown to detect hypoventilation and reduces risk of hypoxia compared to pulse-ox alone
Upon administering the medications and throughout the procedural sedation, you should periodically assess the depth of sedation through tactile stimulation and verbal commands. Full monitoring should continue post-procedure until the patient is at baseline mental status, has appropriate response to verbal stimuli, and is ambulatory at baseline. If any reversal agent is administered, the patient must be observed for full duration of action of the reversal agent.
EtCO2 rising -- decreased minute ventilation 2/2 decreased RR (bradypnea) → CO2 concentration increases
EtCO2 falling or absent -- obstruction (relaxed airway muscle tone) or decreased respiratory drive/tidal volume (hypopnea)
An EtCO2 waveform resembling a shark fin is indicative of severe obstruction -- concerning for bronchospasm!
Sources
Eberson, Craig P., Raymond Y. Hsu, and Todd R. Borenstein. "Procedural sedation in the emergency department." JAAOS-Journal of the American Academy of Orthopaedic Surgeons 23.4 (2015): 233-242.
American Society of Anesthesiologists. "Continuum of depth of sedation: definition of general anesthesia and levels of sedation/analgesia." (2009).
Homma, Yosuke, et al. "A mini‐review of procedural sedation and analgesia in the emergency department." Acute Medicine & Surgery 7.1 (2020): e574.
Bellolio, M. Fernanda, et al. "Incidence of adverse events in adults undergoing procedural sedation in the emergency department: a systematic review and meta‐analysis." Academic Emergency Medicine 23.2 (2016): 119-134.
http://www.emdocs.net/top-10-errors-of-procedural-sedation-in-the-emergency-department/
Gregers, Mads Christian Tofte, et al. "Ketamine as an anesthetic for patients with acute brain injury: a systematic review." Neurocritical care (2020): 1-10.