Getting Under The Skin: Approach to Antibiotic Selection for Cellulitis
Written By: Brian Smith, DO; Edited By: Timothy Khowong, MD
Introduction:
Cellulitis is a common pathology all emergency physicians will undoubtably encounter throughout their careers. So let’s say you have an otherwise healthy patient with normal vital signs who presents to the ED with left lower extremity swelling; you diagnose the patient with cellulitis and you prescribe antibiotics. But, before we get started with this RAMER post I want you to consider a few questions:
With so many options to choose from, how do you decide which antibiotic regimen to prescribe your patient?
Do you prescribe IV or oral antibiotics?
For how long do you prescribe your antibiotic regimen?
Do you cover for MRSA?
What is the evidence to support your answers to questions 1-4?
In this post, we will highlight the evidence (or lack thereof) to support the superiority of specific antibiotic regimens over others for treatment of cellulitis and will make our suggestions for how to best approach antibiotic selection for your patient with uncomplicated cellulitis.
But first, here’s a quick background on cellulitis…
Background:
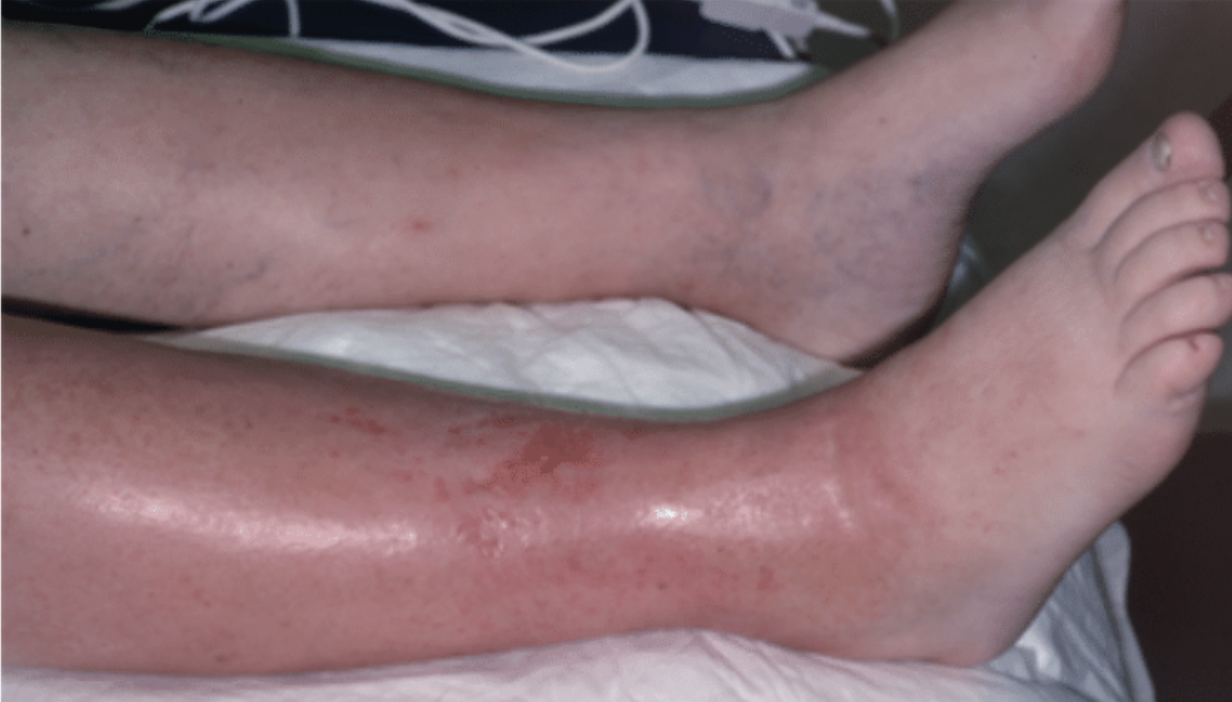
Epidemiology and Clinical Features: Cellulitis - defined as an infection of the dermis and subcutaneous tissues of the skin - accounts for approximately 1.3% of ED visits annually. It can be recognized by tenderness, warmth, erythema, and swelling to the affected area.
Microbiology and Risk Factors: Approximately 80% of cellulitis cases are caused by gram-positive bacteria, with Group A Beta-hemolytic Streptococcus and Methicillin-Resistant Staph aureus (MRSA) being the most common causes of non-purulent and purulent cellulitis, respectively. However, there are various other bacteria that need to be considered as the cause of cellulitis under specific circumstances.
Diagnosis and Treatment: Diagnosis of cellulitis is clinical. The treatment is antibiotics; but what is the most appropriate antibiotic choice, route of administration, and duration of treatment for cellulitis?
Image 1 (left): Anatomy of epidermis, dermis, and subcutaneous tissue. Image 2 right): Clinical features of cellulitis.
Figure 1 (left): General risk factors for cellulitis. Figure 2 (right): Risk factors for specific bacterial etiologies of cellulitis.
The Evidence
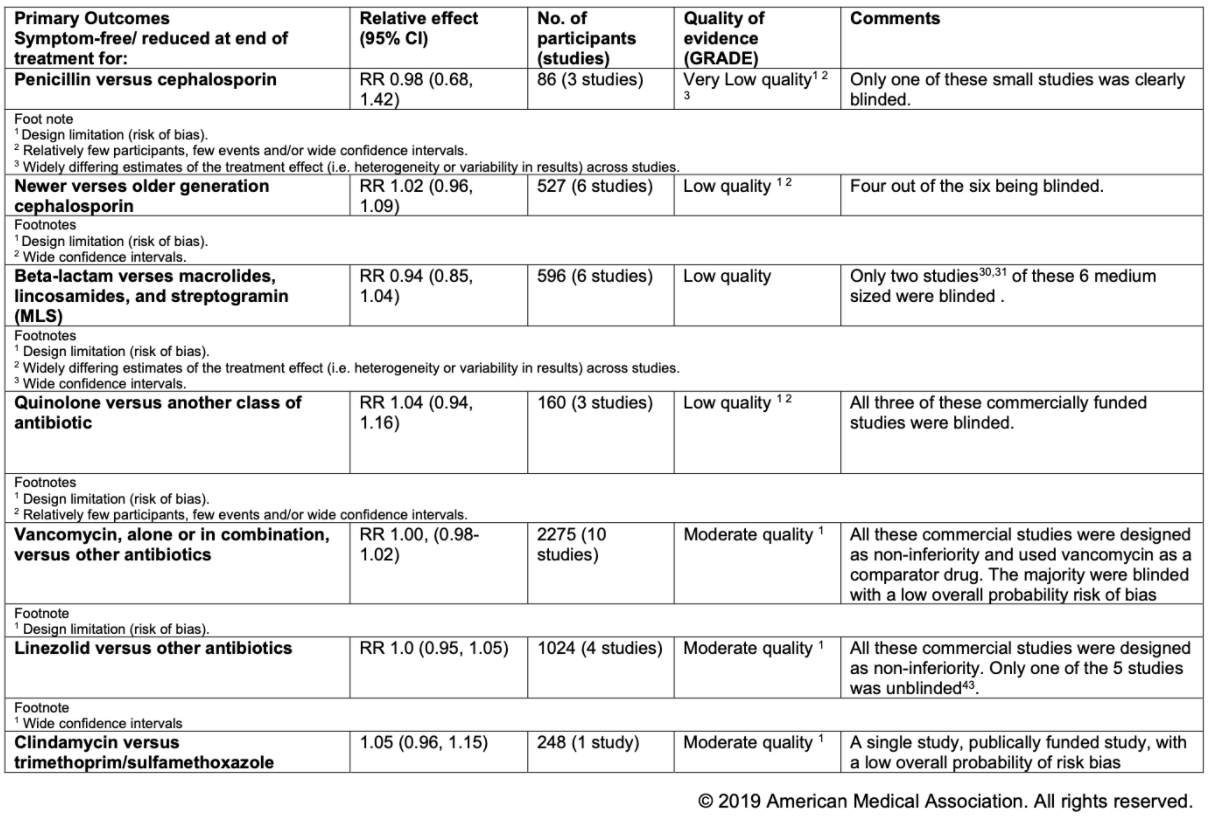
Luckily, Brindle et al. had this same question. In their 2019 article, “Assessment of Antibiotic Treatment of Cellulitis and Erysipelas: A Systematic Review and Meta-analysis”, Brindle et al conducted a systematic review for 43 studies that included 5999 patients to evaluate for evidence of superiority of specific antibiotics over others, IV vs oral antibiotics, and short vs long course of antibiotics in treatment of cellulitis; and their findings may make you jump out of your skin….
The authors found:
There was NO EVIDENCE to support the superiority of one antibiotic over another
There was NO EVIDENCE to support the superiority of IV over oral antibiotics
There was NO EVIDENCE to support the superiority of long-term treatment courses over short-term treatment courses (5 days)
There was NO EVIDENCE to support the superiority of adding MRSA coverage in antibiotic regimen for non-purulent cellulitis.
TL;DR, the authors’ findings can be summarized by this emoji
Figure 3 and 4 (above): Summary of Findings for the Main Comparisons: “Assessment of Antibiotic Treatment of Cellulitis and Erysipelas: A Systematic Review and Meta-analysis”
There are a few caveats that need to be addressed. First, these findings apply to initial treatment of uncomplicated cellulitis: it does not apply to sepsis, necrotizing fasciitis, bite wounds, cellulitis refractory to outpatient therapy.
Second, there were several limitations, specifically regarding differences between the methodologies of studies the authors compared and limitations of the individual studies themselves. These included:
Lack of standard endpoint: Most of the included studies lacked consistent, clear, and precise end points for cellulitis therapies, making comparison between treatments difficult.
Difference between exclusion criteria: some studies either did not specify or did not exclude participants who had received previous antibiotic therapy and included people who did not respond to community treatment. In contrast, 17 studies excluded participants who had received antibiotics before enrollment, although the exclusion period varied between studies.
Blinding and sample size: A number of studies did not adequately explain the process of allocation concealment or blinding, and only more recent studies provided sample size calculations
So I know what you’re thinking: “Great, thanks Brian. You made me read this far and now, after all this, we’re left with the same question… How do I choose which antibiotic regimen to prescribe to a patient with cellulitis”
Approach to Antibiotic Selection for Uncomplicated Cellulitis
As the saying goes, “there are many ways to skin a cat”; and, as this meta-analysis highlighted, there too are many choices for antibiotic regimens for uncomplicated skin infections. So with seemingly countless options, how do you select the best antibiotic regimen for your patient? There are 3 factors your should consider:
Patient Adherence: This may sound obvious, but antibiotics are much more likely to be effective if patients take them as prescribed. To improve chances of adherence, consider shorter course of antibiotics with less frequency of dosing and less severe side effect profiles.
Cost: This factor is especially salient for uninsured patients and those with lower household incomes. If you are unsure of how much a drug costs, one site I’ve found incredible helpful and user-friendly for comparing drug prices is https://www.goodrx.com/
Local Resistance: Certain bacteria in your area can be particularly resistant or sensitive to specific antibiotics. Luckily, we have antibiograms that can help guide our decision-making regarding antibiotic selection. The New York-Presbyterian/Queens antibiograms can be difficult to find, so I’ve provided the link below along with the antibiograms from 2020.
https://infonetqueens.nyp.org/ID/Pages/AntibiogramByPopulationLocation.aspx **
** Note: This link only works when logged in with your CWID
Figures 5-10: New York-Presbyterian/Queens Antibiograms for adult ED, pediatrics, adult inpatient, and Silvercrest nursing home. Note Streptococcus species are not included, as they are typically pan-sensitive in our area.
My Recommendation
I have no skin in the game, but when considering the above factors here are my recommendations for uncomplicated cellulitis treatment at our hospital:
Non-purulent cellulitis: 5-day course of PO Cephalexin 500 mg q6
Sensitivity: Non-purulent cellulitis is most likely to be caused by beta hemolytic streptococcus species. Although it is not shown in the antibiogram, these bacteria are highly sensitive to first generation cephalosporins in our area.
The Evidence: While Cephalexin does not provide MRSA coverage, there was high-quality evidence that patients with non-purulent cellulitis did not benefit with MRSA-active over non MRSA-active antibiotics. Also, the authors of the meta analysis found no difference between treatment with older generation cephalosporin vs newer generation cephalosporin.
The Cost: A 5-day course of Cephalexin is relatively inexpensive, with 20 500 mg tablets costing around $8-15.
Purulent cellulitis: 5-day course of TMP/SMX DS 1 tab PO BID:
While beta-hemolytic strep species in our area are typically pan-sensitive, MRSA is not. Given purulent cellulitis is most likely to be caused by MRSA, it is important to provide MRSA coverage. In our area, MRSA has higher sensitivity to TMP/SMX than other commonly prescribed drugs for cellulitis, such as clindamycin. The TMP/SMX is also inexpensive, with 10 tablets costing around $4-8.
But if you choose a different antibiotic, it's no skin off my back.
References:
Brindle, Richard, et al. “Assessment of Antibiotic Treatment Of Cellulitis And Erysipelas.” JAMA Dermatology, vol. 155, no. 9, 2019, p. 1033., doi:10.1001/jamadermatol.2019.0884.
Kelly, Elizabeth W, and David Magilner. “Chapter 152: Soft Tissue Infections.” Tintinalli's Emergency Medicine: A Comprehensive Study Guide, McGraw-Hill Education, 2020.
Spelman, Denis, and Larry Baddour. “Cellulitis and Skin Abscess in Adults: Treatment.” Uptodate, www.uptodate.com/contents/cellulitis-and-skin-abscess-in-adults-treatment#!