PlexUS Block
Author: Steven Chen MD Editor: Jeffrey Greco MD
Case
35yo M with no PMH who presents to your community ED in the middle of the night after MVC. Patient was the restrained driver and was T-boned on driver’s side by another vehicle going at about 30mph. Airbag deployed, no LOC. On arrival, HR 92, BP 120/80, RR 18, O2 99% on room air and GCS of 15. Patient complaining of severe LUE pain with obvious deformity. Patient is stable and X rays obtained (see images below). Orthopedics attending consulted but would not be able to come in for another hour. Patient is asking for pain medication. You have an ultrasound machine and some lidocaine, what do you do?
Background
Why not do an ultrasound guided supraclavicular brachial plexus block?
-This regional block is often done in upper extremity surgeries to provide adequate anesthesia to upper arm, elbow, forearm, and hand.3
-It will allow for any orthopedic manipulation, splinting, and large laceration repairs without risk of procedural sedation or excessive local anesthetic use.
-This nerve block does not provide reliable anesthesia to the shoulder.3-4
-Shorter length of stay in the ED vs procedural sedation.,5
-High success rate of adequate anesthesia with low complication rate. In one study of 510 consecutive cases performed by 47 different operators at different level of trainings, anesthesia was achieved in 94.6% patient after a single attempt.6
-Potential complications include pneumothorax, vascular puncture, transient ipsilateral diaphragmatic paresis (proximal spread of anesthetic to phrenic nerve), and transient Horner syndrome (anesthetic extending proximally to sympathetic afferents).4
Anatomy
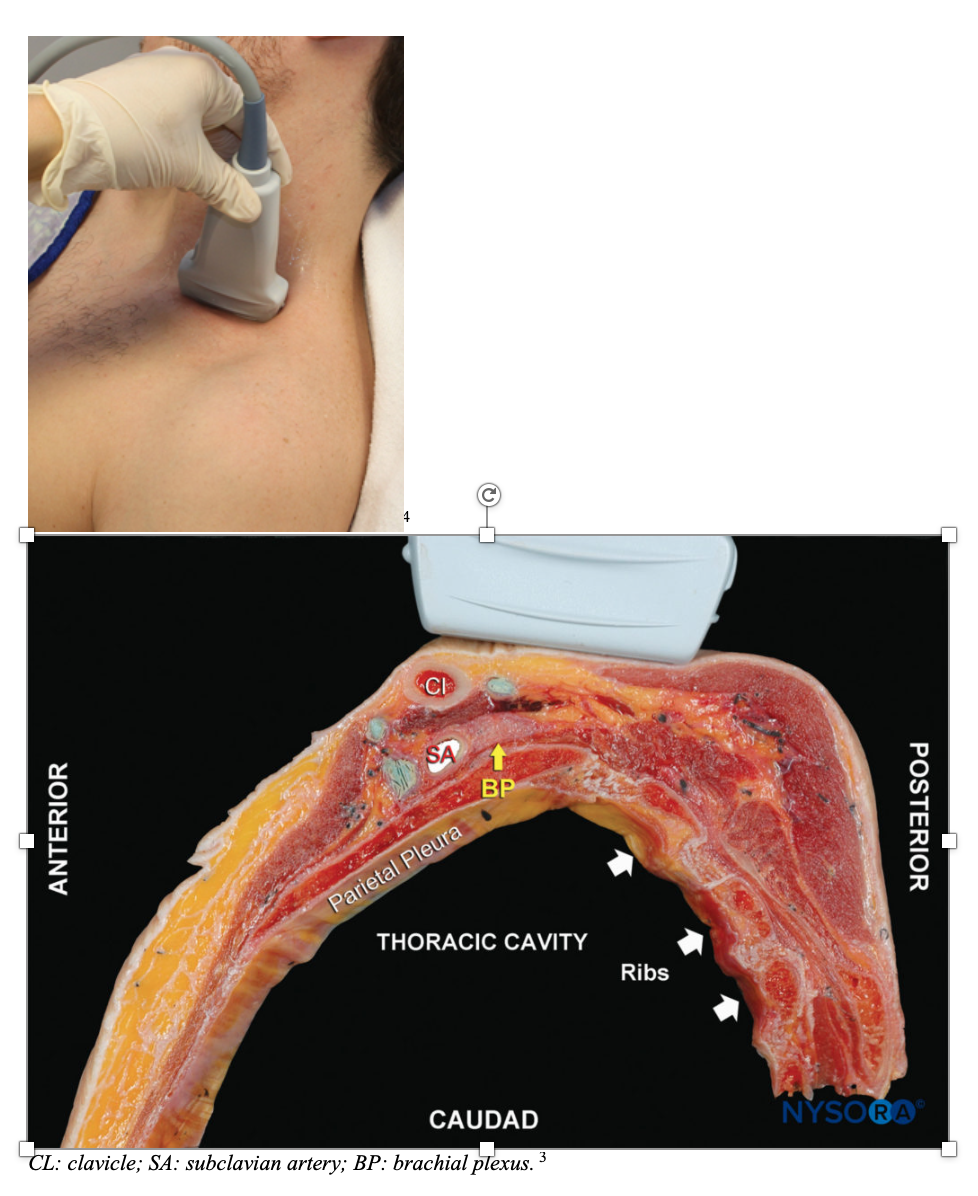
The brachial plexus traverse between the anterior and middle scalene muscle into the supraclavicular fossa, a triangular depression on the lateral neck. In the fossa, subclavian artery will course anterior to the brachial plexus. Together, the subclavian artery and the brachial plexus will course infero-laterally through the fossa, pass under the mid-clavicle, and superior lateral to the first rib as they exit the fossa.3-4
Patient & Probe Positioning
-Place the patient in any positions from recumbent to sitting up right.3-4
-Use a linear probe for better visualization of superficial structures.
-Place the probe in the supraclavicular fossa and orient it perpendicular to the subclavian artery to visualize the brachial plexus, clavicle, subclavian artery, first rib, and pleura all in one view.
-Point the indicator towards the clavicle for a left sided block, and towards the trapezius for a right sided block.3-4
Ultrasound Anatomy
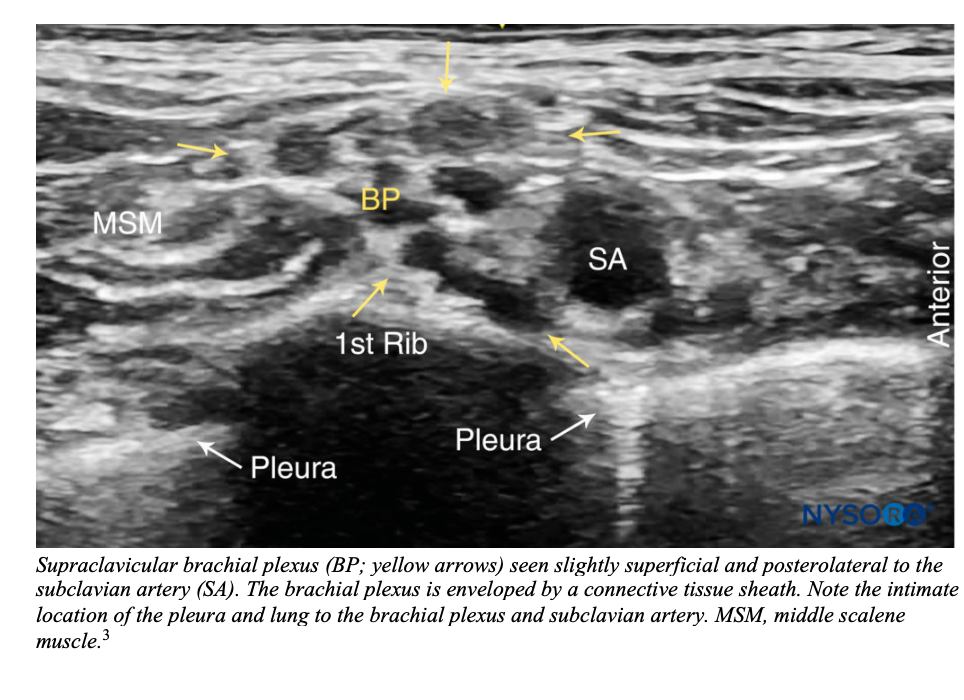
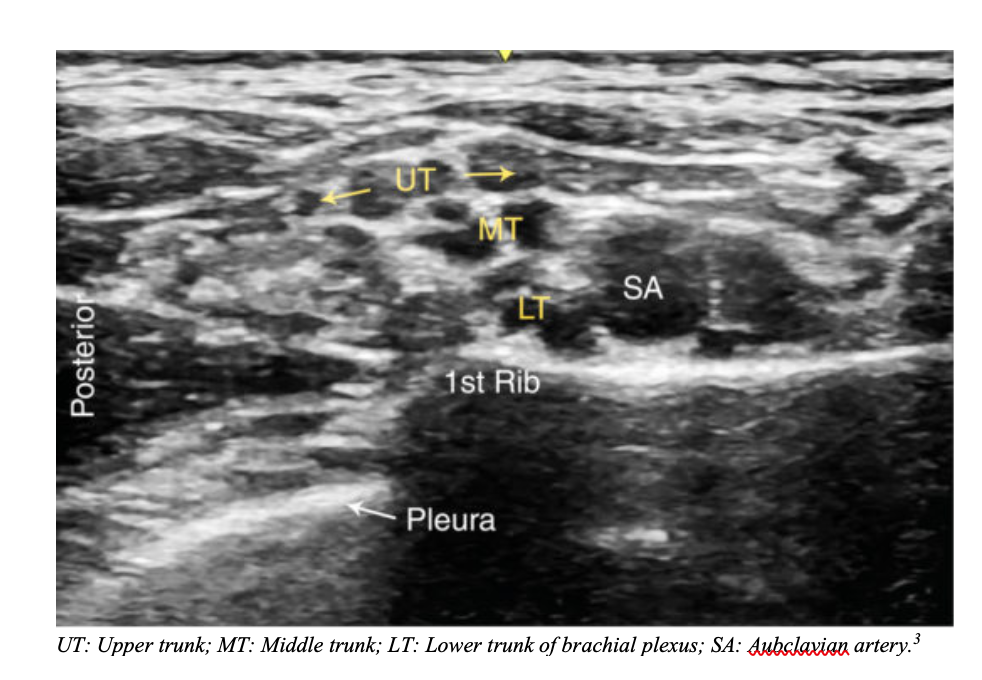
Identify the subclavian artery as an anechoic pulsating structure. The brachial plexus is seen immediately superior and posterior-lateral to the artery as a group of small hyperechoic circles with hypoechoic centers (honeycomb appearance). Obtain the view where the brachial plexus is traversing over the first rib. Hyperechoic pleural lines should be seen anterior and posterior to the first rib.3-4
Subclavian vein is inferior-medial to the subclavian artery but may not always be visualized.4
Be aware that other vessels (dorsal scapular artery, transverse cervical artery, suprascapular artery) can sometime traverse in the vicinity or through the brachial plexus. Be sure to fan through the supraclavicular fossa and use color doppler often to identify these vessels.3
Supraclavicular Block:
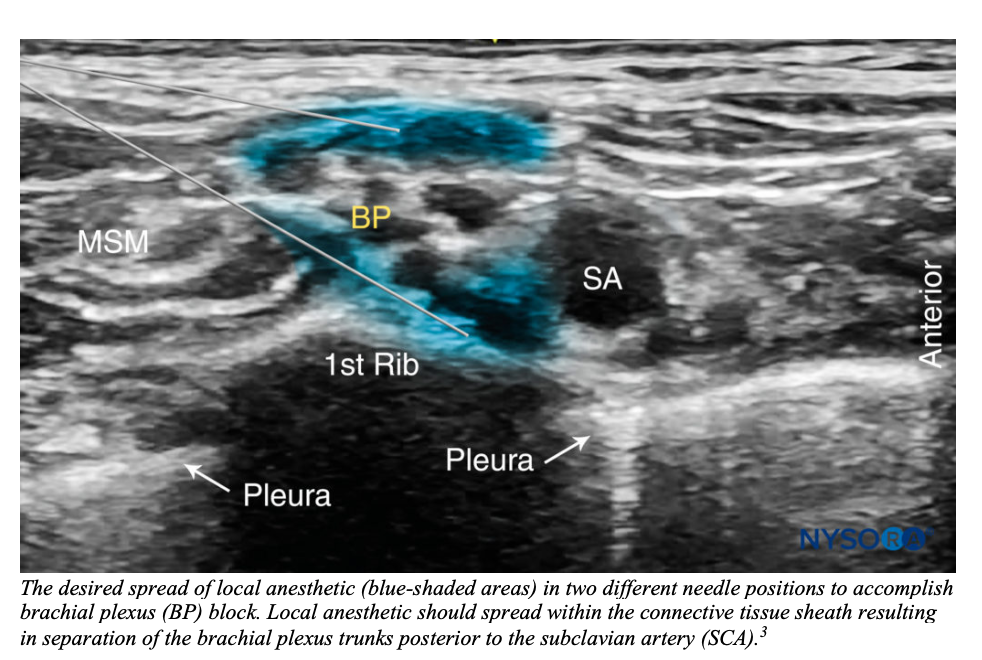
-Goal is to place the needle into the brachial plexus sheath and surround the trunks and division of the plexus with local anesthetics.3
-Sterilely prep the insertion site.
-Use a 25-27 gauge needle and use the in-plane longitudinal approach where the needle and ultrasound probe are in the same orientation. The needle tip should be visualized throughout the procedure.3-4 -Insert the needle into the brachial plexus sheath (often associated with a palpable pop) but never directly into the plexus. Inject 1-2 ml of local anesthetic to ensure proper needle placement.3-4
-Appropriate needle placement is confirmed by sonographic evidence of spread of anesthetic around the brachial plexus.3-4,9
-To ensure complete block, the plexus needs to be surrounded by anesthetic. This will require re-entry of needle into the brachial sheath. Two common initial injection points are superior and inferior to the brachial plexus. The needle should be redirected as needed to ensure the entire plexus is surrounded by anesthetic.3-4,9
-20-40ml of anesthetics are enough for an adequate block.3-4
Tips:
-Make sure to get a view of brachial plexus traversing over the first rib. That way, if the needle was inadvertently inserted past the brachial plexus, it would hit the rib instead of causing a pneumothorax.9
-Can inject small volumes of anesthetic to visualize needle tip as it is inserted through various tissue layers (termed hydrodissection).3-4,9
-Fan and use color doppler often to avoid puncturing vasculatures in the vicinity.
References
1. https://aminoapps.com/c/sfx/page/blog/simple-arm-lacerations/eBKM_VkI3udYQvJklqYEZ1dR6xJg4Y3GqW
2. https://www.orthobullets.com/
3. Ultrasound-guided supraclavicular brachial plexus block. NYSORA. https://www.nysora.com/regional-anesthesia-for-specific-surgical-procedures/upper-extremity-regional-anesthesia-for-specific-surgical-procedures/anesthesia-and-analgesia-for-elbow-and-forearm-procedures/ultrasound-guided-supraclavicular-brachial-plexus-block/ Accessed September 27, 2019.
4. Bunting L. Supraclavicular brachial plexus block. ACEP – Sonoguide. https://www.acep.org/sonoguide/supraclavicular_plexus_block.html. Accessed September 27, 2019
5. Stone MB, Wang R, Price DD. Ultrasound-guided supraclavicular brachial plexus nerve block vs procedural sedation for the treatment of upper extremity emergencies. Am J Emerg Med. 2008;26(6):706-10.
6. Perlas A, Lobo G, Lo N, Brull R, Chan VW, Karkhanis R. Ultrasound-guided supraclavicular block: outcome of 510 consecutive cases. Reg Anesth Pain Med. 2009;34(2):171-6.
7. Neal JM, Gerancher JC, Hebl JR, et al. Upper extremity regional anaesthesia: essentials of our current understanding, 2008. Reg Anaesth Pain Med 2009;34(2):134-170.
8. http://www.mountainhp.ca/conditions-treated/what-is-thoracic-outlet-syndrome/
9. Avila, J. Supraclavicular nerve block. 5MinSono. http://5minsono.com/supraclav/ Accessed September 27, 2019.